22 Addiction and Substance Use
Alexandria Lewis

I. Human Development, Diversity, and Behavior in the Environment
IA. Human Growth and Development
KSAs:
– The effects of addiction and substance abuse on individuals, families, groups, organizations, and communities
– Addiction theories and conceptsII. Assessment and Intervention Planning
IIA. Biopsychosocial History and Collateral Data
KSAs: The indicators of addiction and substance abuse
Important Note: The ASWB started using the DSM 5 TR in January 2024.
overview
Human cultures have used psychoactive substances for various purposes, including religious ceremonies, medicinal healing, to experience altered mind states, and for the pure pleasure it can produce. Keeping a broad view of substance use is key.
Addiction Defined (American Society of Addiction Medicine)
Addiction is a primary, chronic disease of brain reward, motivation, memory and related circuitry. Dysfunction in these circuits leads to characteristic biological, psychological, social and spiritual manifestations. This is reflected in an individual pathologically pursuing reward and/or relief by substance use and other behaviors.
Addiction is characterized by inability to consistently abstain, impairment in behavioral control, and craving, diminished recognition of significant problems with one’s behaviors and interpersonal relationships, and a dysfunctional emotional response. Like other chronic diseases, addiction often involves cycles of relapse and remission. Without treatment or engagement in recovery activities, addiction is progressive and can result in disability or premature death.
The following is a good brief video about the reward circuit and how the brain responds to natural rewards and drugs.
This is a good animated video that provides a visual about how the brain responds to addictive substances:
Resource
Reward Pathway in the Brain (Khan Academy)
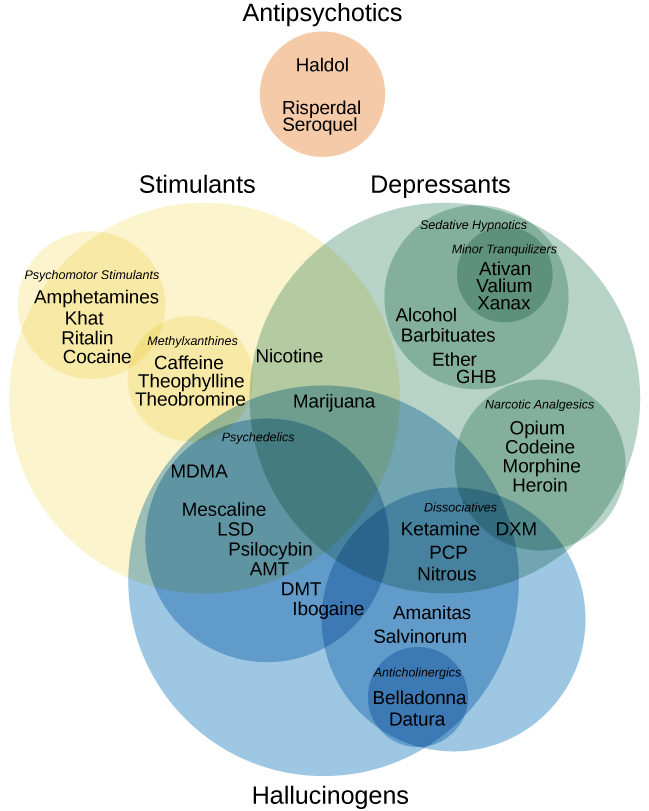
10 Separate Classes of Drugs:
- Alcohol
- Caffeine
- Cannabis
- Hallucinogens
- Inhalants
- Opioids
- Sedatives, Hypnotics, and Anxiolytics
- Stimulants
- Tobacco
- Other substances
Substance-related disorders are divided into two groups:
- Substance use disorders
- Substance-induced disorders
- Examples: Intoxication, withdrawal, and other substance/medication-induced mental disorders (e.g., psychotic disorders, bipolar and related disorders, depressive disorders).
Note: Tolerance nor withdrawal are necessary for a diagnosis of a substance use disorder. All classes of drugs do not have withdrawal symptoms.
Note: Click the drop down icon.
Diagnostic Criteria Highlights
Criterion A: A problematic pattern of substance use leading to clinically significant impairment or distress, as manifested by at least two of the following, occurring within a 12-month period.
| Criterion | Description |
| A (1) | Takes the substance in larger amounts or over a longer period of time than was originally intended. |
| A (2) | Expresses a persistent desire to cut down or regulate use and may report multiple unsuccessful efforts to decrease or discontinue use. |
| A (3) | May spend a great deal of time obtaining the substance, using the substance, or recovering from its effects. |
| A (4) | Intense desire or urge that may occur at any time but is more likely when in an environment where the drug previously was obtained or used (craving). |
| A (5-7) | Social impairment. |
| A (8-9) | Risky substance use. |
| A (10) | Tolerance. |
| A (11) | Withdrawal. |
After full criteria for the substance use disorder were previously met, specify if:
- In early remission:
- None of the criteria for the substance use disorder have been met for at least 3 months but for less than 12 months (with the exception that Criterion A4, “Craving, or a strong desire or urge to use alcohol,” may be met).
- In sustained remission:
- None of the criteria for the substance use disorder have been met at any time during a period of 12 months or longer (with the exception that Criterion A4, “Craving, or a strong desire or urge to use alcohol,” may be met).
Controlled Environment:
- Use when access to the substance is restricted.
Contrasting Withdrawal Symptoms
Note: To advance to the next slide, click the arrow at the bottom of the slide presentation.
Contrasting Intoxication Criteria
Resource
Alcohol-Related Disorders
– Alcohol Use Disorder
– Alcohol Intoxication
– Alcohol Withdrawal
– Other Alcohol-Induced Disorder
– Unspecified Alcohol-Related Disorder
Self-Check
Alcohol Use Disorder
Alcohol Intoxication
Note: Click the drop down icon.
Alcohol Withdrawal
Note: Click the drop down icon.
| Condition | Description | Symptoms |
| Wernicke-Korsakoff Syndrome | These neurological syndromes are considered elements of the same disease and are common in folks with chronic alcohol use problems. Wernicke’s encephalopathy results in brain damage to the hypothalamus and thalamus from a lack of thiamine (vitamin B). Korsakoff syndrome is a memory disorder and is sometimes referred to as Korsakoff’s amnesic syndrome. These symptoms are reversible if caught before further brain damage, and the treatment is thiamine, hydration, and nutrition. | Wernicke’s encephalopathy: Lack of muscle coordination (ataxia), hypothermia, vision problems, confusion, low blood pressure, and coma. Korsakoff syndrome: Amnesia, disorientation, tremor, vision problems, and coma. |
| Delirium Tremens (DT) | DT is a severe form of alcohol withdrawal in people with a history of chronic alcohol use and is rare. | Delirium tremens: Hallucinations, agitation, body tremors, mental status changes, rapid mood changes, fatigue, and fear, to name several symptoms. |
Caffeine-Related Disorders
– Caffeine Intoxication
– Caffeine Withdrawal
– Other Caffeine-Induced Disorder
– Unspecified Caffeine-Related Disorder
Note: Click the drop down icon.
Cannabis-Related Disorders
– Cannabis Use Disorder
– Cannabis Intoxication
– Cannabis Withdrawal
– Other Cannabis-Induced Disorders
– Unspecified Cannabis-Related Disorder
Hallucinogen-Related Disorders
– Phencyclidine (PCP) Use Disorder
– Other Hallucinogen Use Disorder
– PCP Intoxication
– Other Hallucinogen Intoxication
– Hallucinogen Persisting Perception Disorder
– Other PCP-Induced Disorder
– Other Hallucinogen-Induced Disorder
– Unspecified PCP-Related Disorder
– Unspecified Hallucinogen-Induced Disorder
Withdrawal and PCP
PCP Intoxication
Note: Click the drop down icon.
Other Hallucinogen Use Disorder
Inhalant-Related Disorders
– Inhalant Use Disorder
– Inhalant Intoxication
– Other Inhalant-Induced Disorder
– Unspecified Inhalant-Related Disorder
Highlights
- Examples of inhalants: Glue, shoe polish, gasoline, lighter fluid, or spray agents.
- 10% of 13-year-olds report the use of inhalants (at least one time).
- Tolerance and mild withdrawal are each reported by about 10% of individuals who use inhalants, and a few individuals use inhalants to avoid withdrawal.
- Withdrawal is not recognized as a diagnostic criterion because withdrawal symptoms are considered mild.
- About 0.4% of Americans ages 12–17 years have a pattern of use that meets criteria for inhalant use disorder in the past 12 months.
- Deaths from inhalants can occur from aspiration of vomitus, asphyxiation, respiratory problems, arrhythmias, or accidents. Using inhalants in a closed container (plastic bag) can lead to death.
Opioid Use Disorder
– Opioid Use Disorder
– Opioid Intoxication
– Opioid Withdrawal
-Other Opioid-Induced Disorders
– Unspecified Opioid-Related Disorder
- Opiates: Naturally occurring substances derived directly from the opium poppy plant. Examples include morphine and codeine. These drugs have been used for many centuries for their analgesic, sedative, and euphoric properties.
- Opioids: Broader term that includes all substances, both natural and synthetic, that bind to opioid receptors in the brain (including those not derived from the opium poppy). This includes natural opiates like morphine, semi-synthetic opioids made from opiates such as oxycodone and hydrocodone, and fully synthetic opioids like fentanyl and methadone.
Note: All opiates are opioids, but not all opioids are opiates.
Medications for Opioid Use (NIDA/NIH) YouTube Video
DSM 5 Checklist for Opioid Use Disorder
Sedative, Hypnotic, or Anxiolytic-Related Disorders
Sedative, Hypnotic, or Anxiolytic-Related Disorders
– Sedative, Hypnotic, or Anxiolytic Use Disorder
– Sedative, Hypnotic, or Anxiolytic Intoxication
– Sedative, Hypnotic, or Anxiolytic Withdrawal
– Other Sedative-, Hypnotic-, or Anxiolytic-Induced Disorders
– Unspecified Sedative-, Hypnotic-, or Anxiolytic-Related Disorder
Note: Click the drop down icon.
Stimulant-Related Disorders
Stimulant-Related Disorders
– Stimulant Use Disorder
– Stimulant Intoxication
– Stimulant Withdrawal
– Other Stimulant-Induced Disorders
– Unspecified Stimulant-Related Disorder
Drugs that have similar effects:
- Dexmethylphendiate
- Example: Focalin XR (dexmethylphenidate hydrochloride) is a mild central nervous system (CNS) stimulant used to treat attention deficit hyperactivity disorder (ADHD).
- Phendimetrazine (appetite suppressant)
- Cocaine
- Crack
- Khat (plant)
Persons who use stimulants may use other substances with properties that sedate as a way to reduce negative symptoms of stimulants, such as nervousness and insomnia.
Tobacco-Related Disorders
Tobacco-Related Disorders
– Tobacco Use Disorder
– Tobacco Withdrawal
– Other Tobacco-Induced Disorders
– Unspecified Tobacco-Related Disorder
Tobacco Use Highlights:
- Similar to opioid use disorder with specifiers, there is a specifier for maintenance therapy (i.e., taking a long-term maintenance medication, and no criteria for tobacco use order have been met for that class of medication except tolerance to, or withdrawal from, the nicotine replacement medication.
- Continued use of tobacco products increases one’s risk of mortality.
- The most commonly used tobacco product is cigarettes.
- Smoking may cause physical health problems like cancers, chronic obstructive pulmonary disease (COPD), coughing, and cardiovascular problems.
- Craving can occur when not smoking for several hours, which leads to people smoking to reduce withdrawal symptoms.
Other (Unknown) Substance-Related Disorders
Other (Unknown) Substance-Related Disorders
– Other (or Unknown) Substance Use Disorder
– Other (or Unknown) Substance Intoxication
– Other (or Unknown) Substance Withdrawal
– Other (or Unknown) Substance–Induced Disorders
– Unspecified Other (or Unknown) Substance–Related Disorder
Examples of some of the substances that could be included in other substance use disorder include:
- Antiparkinsonian medications
- Anabolic steroids
- Antihistamines
- Nitrous oxide (sometimes referred to as laughing gas)
- Amyl-, butyl-, or isobutyl-nitrites gases
Diagnosis: The use of the substance is used in the diagnosis when known. For instance, nitrous oxide disorder.
Non-Substance related disorders
Gambling Disorder
A. Persistent and recurrent problematic gambling behavior leading to clinically significant
impairment or distress, as indicated by the individual exhibiting four (or more) of the following
in a 12-month period:
- Needs to gamble with increasing amounts of money in order to achieve the desired excitement.
- Is restless or irritable when attempting to cut down or stop gambling.
- Has made repeated unsuccessful efforts to control, cut back, or stop gambling.
- Is often preoccupied with gambling (e.g., having persistent thoughts of reliving past gambling
experiences, handicapping or planning the next venture, thinking of ways to get money with which to
gamble). - Often gambles when feeling distressed (e.g., helpless, guilty, anxious, depressed).
- After losing money gambling, often returns another day to get even (“chasing” one’s losses).
- Lies to conceal the extent of involvement with gambling.
- Has jeopardized or lost a significant relationship, job, or educational or career op portunity
because of gambling. - Relies on others to provide money to relieve desperate financial situations caused by gambling.
B. The gambling behavior is not better explained by a manic episode.
Theories of Addiction
Source of some of the following content on addiction theories (biopsychosocial framework): Section 2.8: Ch. 4- Classifying Theories is adapted and shared under a CC BY-NC 4.0 license and was authored, remixed, and/or curated by Audrey Begun.
There are several different theories, models, and perspectives that can be used to examine addiction (Hovarth et al., n.d.):
- Biopsychosocial-spiritual model
- Biological model
- Disease model
- Evolutionary model
- Psychopathological model
- Learning theory
- Social learning theory
- Cognitive theory
- Educational model
- Developmental model
- General systems theory
- Sociocultural model
- Moral model
- Spiritual model
As a reminder, addiction can also occur with activities (e.g., gambling, shopping, sex).
Petrovich and Garcia (2016) identify three major categories that provide explanations about how addictions develop:
- Biological
- Neurobiological
- Genetics
- Psychological
- Cognition
- Behavior
- Psychodynamic
- Personality
- Sociocultural
- Family
- Environment
- Cultural aspects
References:
Hovarth, A.T., Misra, K., Epner, A.K., & Cooper, G.M. (n.d.). Introduction to causes of addiction. Retrieved from http://www.amhc.org/poc/view_doc.php?type=doc&id=48340&cn=1408
Petrovich, A., & Garcia, B. (2016). Strengthening the DSM: Incorporating resilience and cultural competence. Springer Publishing Company, LLC
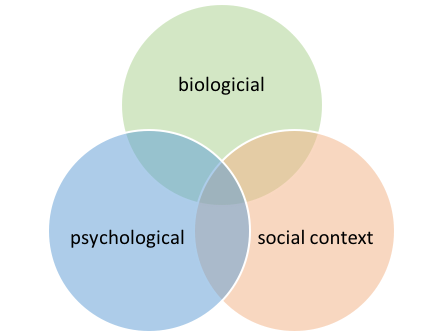
Biopsychosocial Framework
There are three general theory domains that comprise a biopsychosocial framework. This framework can be considered a blended framework since it captures several different models:
- Biological Model
- Psychological Theories
- Social Context
Genetics:
- genetics contribute to both vulnerability and resilience for developing a substance use disorder;
- genetics alone do not establish a person’s destiny: genetic makeup interacts with environment and experience to determine whether or not a substance use disorder emerges; and
- there is no single, specific “addiction gene” that applies to all of the different types of substances—genetic susceptibility or resilience appears to be relatively specific to each different type of substance.
- Learning theory (operant and classical conditioning).
- Social learning theory (observational learning).
- Expectancies theory (a person’s expected outcomes associated with using a substance).
- Information processing (effects of different types of substances on learning, thinking, behaving).
- Psychodynamic & attachment theory (including self-medication theory).
(3) Social Context:
- Ease of access to substances in the social and physical environment.
- Social norms about substance use and misuse expressed in the social environment.
- The role played by experiencing social oppression, discrimination, and exploitation in developing/maintaining substance use and substance use disorders.
- Impact of policy, programs/services, laws, and law enforcement in substance use and misuse.
Moral Model
- Views people as having a lack of willpower and determination to stop using substances.
- Views people as making poor decisions.
- Views people as not deserving of services. For instance, some programs, shelters, etc., will terminate someone if the results of a urinalysis shows the use of substances.
assessment and treatment highlights
The following content about addiction theories is adapted and shared from:
- Foundations of Addiction Studies, licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License, except where otherwise noted.
- Drugs, Health, Addictions & Behaviour – 1st Canadian Edition by Denise Halsey and Sunil Boodhai is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License, except where otherwise noted.
When reading ASWB exam questions, remember the steps of the helping process. Assessment comes before treatment/intervention.
Examples of screening instruments:
In contrast to the screening process, assessment is a longer and more formal process. These tools provide insight into the presence of a problem and set up the next step of looking for helpful programs or interventions to address the problem.
Sample Client
Jessica is a 26-year-old female who recently received her second driving under the influence (DUI) ticket and has been charged with a misdemeanor crime. She got her first DUI at age 21 and lost her license for one year. During that time, she completed a basic risk education DUI course and paid several thousand dollars in fines and attorney’s fees.
Jessica drinks with her friends on weekends, usually having five or six drinks per night. One of Jessica’s best friends growing up (Kaitlin) has started distancing herself from Jessica because she does not like how much their other friends drink. Kaitlin still occasionally invites Jessica to hang out, but Jessica refuses because no drinking is involved.
In addition to alcohol, Jessica has started taking Xanax, a benzodiazepine. Although she has a prescription from her doctor to take Xanax to help treat her anxiety disorder, Jessica often takes more than prescribed, sometimes even mixing the pills with her alcohol consumption.
Jessica works full-time as a graphic designer and does most of her work from home. She says that she has little time to socialize during the week, so she looks forward to the weekend when she can see her friends and relax.
Now that she has a second DUI, Jessica has lost her license again, although she is not overly concerned because she can continue working from home and can walk or order a ride wherever she needs to go.
The court has ordered Jessica to have an evaluation and complete any treatment recommendations.
A screening of Jessica would reveal that she likely meets the criteria for a substance use disorder and should receive a full assessment. (Note that a screening tool alone never diagnoses a substance use disorder.)
Exercise
Consider the story of Jessica in the example above:
- What stands out about her story?
- Identify the substance or substances that might be a problem for Jessica.
- If you were evaluating Jessica, what are some of the questions you would ask her?
- List at least three issues that might be addressed in a treatment plan for Jessica.
- How many of the DSM-5 criteria for Substance Use Disorder (see list below in this chapter) can you identify from the brief description above?
- How do her legal issues impact treatment?
Risk and Protective Factors
Risk factors can be internal (within the individual) or external (outside the individual). No single risk factor or combination of risk factors determines whether a person will develop an addiction. Instead, having one or more risk factors increases the chances that an individual who uses alcohol or other drugs will develop an addiction.
These risk factors include (in no particular order of importance):
- Having a mental health disorder
- Lack of family involvement
- Lower socioeconomic status
- Peer pressure
- Using drugs at an early age
- Chaotic home environment
- Poor social skills
- Substance availability
- Low self-esteem
- Poor academic performance or other school-related problems
- Using substances with a higher likelihood of physical or psychological dependence (opiates, cocaine, etc.)
- Route of administration (such as smoking or injection)
These protective factors include (in no particular order of importance):
- Strong network of support
- Parental/family involvement
- Healthy coping strategies
- Sense of psychological and physical safety
- High self-esteem
- Ability to emotionally self-regulate
- Resiliency
- Social competence
TREATMENT HIGHLIGHTS
Effective treatment should address the individual’s multiple needs, not just their substance use. Treatment must address the whole person.
- Short and long-term residential treatment.
- Outpatient treatment programs.
- Behavioral therapies—including individual, family, or group counseling—are commonly used forms of substance use treatment
- Pharmacotherapies (medication-assisted therapy) can be an essential component of treatment for some clients, especially when combined with counseling and other behavioral therapies.
- Mutual help groups (e.g., 12-step groups). Examples: Alcoholics Anonymous, Al-Anon Family Groups, and Narcotics Anonymous.
Relapse should not be viewed as “failure” because recovery is a process.
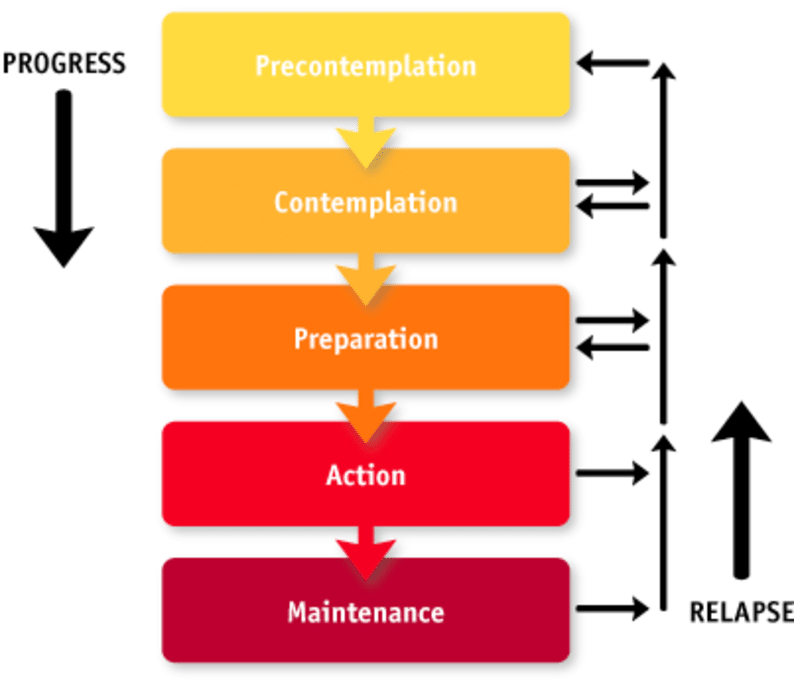
transtheoretical model
People living with a substance use disorder may not be ready to acknowledge their habits, particularly regarding their substance use. Understanding where a person may place themselves on this model is helpful for helping professionals. There is no beginning or end to the stages of change model. People may also skip through stages. Being nonjudgmental and supportive at each stage is essential when using this model