58 Intervention Planning
Alexandria Lewis

Content Outline, Competency, and KSAs
II. Content Outline: Assessment and Intervention Planning
IIB. Competency: Assessment Methods and Techniques
KSAs:
– Methods to involve clients/client systems in intervention planning
– The indicators of motivation, resistance, and readiness to change (available in the Assessment Methods and Techniques chapter)
– Cultural considerations in the creation of an intervention plan
– The criteria used in the selection of intervention/treatment modalities (e.g., client/client system abilities, culture, life stage)
– The components of intervention, treatment, and service plans
– Psychotherapies
– The impact of immigration, refugee, or undocumented status on service delivery
– Discharge, aftercare, and follow-up planning
III. Interventions with Clients/Client Systems
IIIA. Intervention Processes and Techniques for Use Across Systems
– Techniques used for follow-up
– The indicators of client/client system readiness for termination
overview
As a reminder, the ASWB exam questions focus on generalist social work practice questions. Keep in mind generalist social work practice models and the order of the helping process. Consider answer choices that reflect collaboration, respect for autonomy, and collaborative decision-making (client-driven). Avoid choices where the social worker makes decisions for the client without input from the client. This process is the same for micro, mezzo, and macro intervention planning questions.
Methods to involve clients/client systems in intervention planning
Helping Process Overview (Hepworth et al., 2017):
- Phase I
- Exploration
- Engagement
- Assessment
- Planning
- Phase II
- Implementation
- Goal Attainment
- Phase III
- Evaluation
- Termination
Reference: Hepworth, D.H., Rooney, R.H., Rooney, G.D., & Storm-Gottfried (2017). Direct social work practice: Theory and skills. Cengage Learning.
Intervention planning should always prioritize the goals of the client system, even if the client is ‘involuntary.’ Generalist social work practice models emphasize goal setting during the intervention planning process. As part of this process, client/client system should direct the goal-setting process. For instance, the problem/issue is what the client says it is in facilitating the goal-setting process. Social workers should use empathic communication skills, including validation, active listening, open-ended questions, motivational interviewing techniques, etc., to involve client/client systems in intervention planning.
Key Tasks To Consider in Intervention Planning:
-
Collaboratively Define the Problem:
-
Begin with the client’s perspective; the problem is what the client says it is.
-
Use strengths-based language and actively listen to client concerns.
-
-
Engage the Client in Goal-Setting:
-
Encourage the client to identify meaningful, realistic, and measurable goals.
-
Support the client’s autonomy (even in mandated situations) by negotiating shared goals.
-
-
Assess Motivation and Readiness for Change:
-
Use tools like the stages of change model to evaluate where the client stands.
-
Address resistance with empathy and motivational interviewing techniques.
-
-
Identify Barriers and Cultural Considerations:
-
Recognize how cultural identity, immigration status, and systemic factors affect intervention planning.
-
Incorporate cultural strengths and preferences into the plan.
-
-
Select Appropriate Intervention/Treatment Modalities:
-
Base choices on client needs, culture, developmental stage, and resources.
-
Be familiar with a range of modalities (CBT, task-centered practice, family therapy, etc.).
-
-
Develop a Clear, Written Service Plan:
-
Include goals, objectives, timelines, roles, and methods.
-
Ensure the plan is specific, measurable, achievable, relevant, and time-bound (SMART).
-
-
Review and Adjust the Plan Collaboratively:
-
Involve the client in ongoing monitoring and revisions.
-
Stay flexible to adapt interventions as new needs emerge.
-
-
Plan for Discharge and Follow-Up:
-
From the start, consider long-term needs and support systems.
-
Ensure continuity of care and client autonomy post-intervention.
-
Self-Check
Cultural considerations in the creation of an intervention plan
Consider answer choices to intervention planning questions that reflect and respect client/client systems’ cultural layers (e.g., values, language, norms, beliefs, and worldview).
Cultural Consideration Examples:
-
Beliefs about help-seeking (e.g., stigma or mistrust of mental health systems).
-
Family roles, collectivism vs. individualism.
-
Religion or spirituality.
-
Language and communication preferences.
- Communication styles (direct vs. indirect communication).
-
Experiences of marginalization, discrimination, or immigration-related trauma.
- Time orientation (present-focused vs. future-oriented).
- Health beliefs (traditional healing practices and beliefs about the cause of illnesses).
- Gender roles (cultural expectations).
- Decision-making practices (elder in the family, family as a unit).
Examples of Implications for Planning:
- Communication styles: Be aware of one’s own communication style and how that can impact clients. Adjust engagement strategies to reflect preferred communication norms.
- Time orientation: May affect goal-setting, timeliness, or perceptions of ‘urgency.’
- Decision-making practices: Collaborate accordingly. May need to include family or community leaders in planning.
- Language: Adapt documentation, use visuals or oral formats for planning and follow-up, etc.
- Historical/intergenerational trauma: May impact trust in systems, readiness for change, or perceived relevance of services.
Self-Check
The criteria used in the selection of intervention/treatment modalities
When you encounter an exam question about intervention planning, remember to consider the broader context, including client needs, cultural relevance, appropriateness of the modality, and ethical standards, before selecting the answer choice.
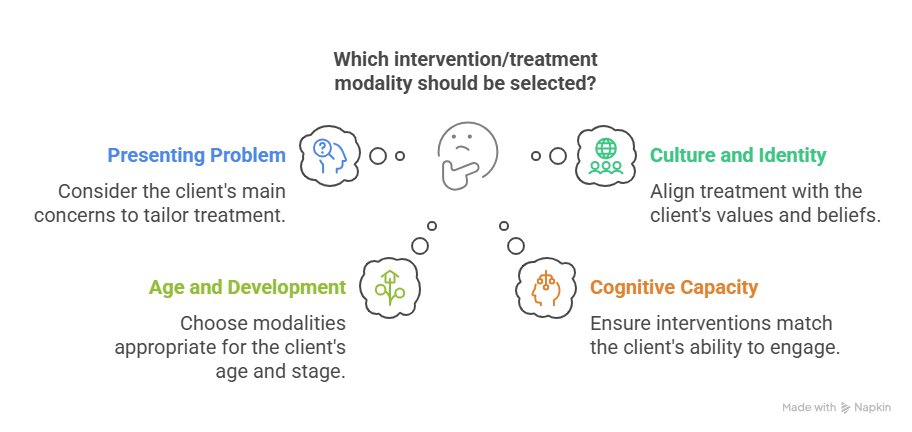
Accessible Image Description:
Client Factors:
-
Presenting Problem(s): What are the client’s main concerns? (e.g., trauma, anxiety, family conflict)
-
Culture and Identity: How do the client’s values, beliefs, or identity inform treatment preferences?
-
Age and Developmental Stage: Some modalities (e.g., play therapy) are appropriate only for certain populations.
-
Cognitive Capacity or Functional Level: Interventions must be appropriate for a client’s ability to engage.
Examples of Modalities and When They Might Be Selected:
| Modality | Best Used When… |
|---|---|
| Task-Centered Practice | Client wants a brief, structured approach focused on solving specific problems in a set timeframe |
| Trauma-Focused Cognitive Behavioral Therapy (TF-CBT) | Client is a child or adolescent with a trauma history and needs structured support |
| Eye Movement Desensitization and Reprocessing (EMDR) | Client is experiencing symptoms of trauma or PTSD and is open to non-traditional approaches |
| Family Systems Therapy | The problem is rooted in family dynamics or intergenerational patterns |
| Psychoeducation | Client or family needs to understand a diagnosis, condition, or process (e.g., coping with schizophrenia) |
| Supportive Therapy | Client is in crisis, experiencing grief, or adjusting to a major life event. |
| Group Therapy | Client would benefit from shared experiences, peer support, and collective insight |
| Play Therapy | Client is a child and may not be able to verbalize emotions directly |
| Cognitive Behavioral Therapy (CBT) | Client wants a structured, goal-oriented approach to change thoughts/behaviors |
| Dialectical Behavior Therapy (DBT) | Client has emotional regulation or interpersonal difficulties (often with borderline personality disorder) |
| Narrative Therapy | Client’s identity and cultural story are central; strength-based focus preferred |
| Solution-Focused Brief Therapy | Client is goal-oriented and prefers a short-term, practical approach |
| Acceptance and Commitment Therapy (ACT) | Client avoiding difficult emotions, managing chronic conditions, or seeking values-based living despite ongoing distress. Useful for anxiety, depression, trauma, chronic pain, or substance use. |
| Rational Emotive Behavior Therapy (REBT) |
Clients need help identifying and challenging irrational beliefs that lead to emotional distress. Common for issues like anxiety, anger, and self-defeating thought patterns. Focuses on changing core beliefs using logic and disputation |
| Internal Family Systems (IFS) |
Clients working through trauma, internal conflict, or complex emotional patterns. Focuses on exploring and healing “parts” of the self (e.g., inner child, protector) in a non-pathologizing way. Helps clients build self-leadership and inner harmony. |
| Psychodynamic Therapy |
Clients exploring longstanding emotional patterns, relationship dynamics, or unconscious motivations. Focuses on insight, self-awareness, and how early experiences shape current behavior. Often used for depression, anxiety, and relational issues. |
With treatment fit, consider empirical support, client preferences, and prior interventions. For instance, prior interventions that have worked or not worked for the client. The client is the center of the selection of treatment modalities. Remember that it is not solely about ‘evidence-based’ intervention.
In reality, there will be contextual and systemic considerations regarding treatment modalities, such as legal/ethical requirements, service setting, and agency resources. Even the type of insurance a client has can impact the number of treatment sessions.
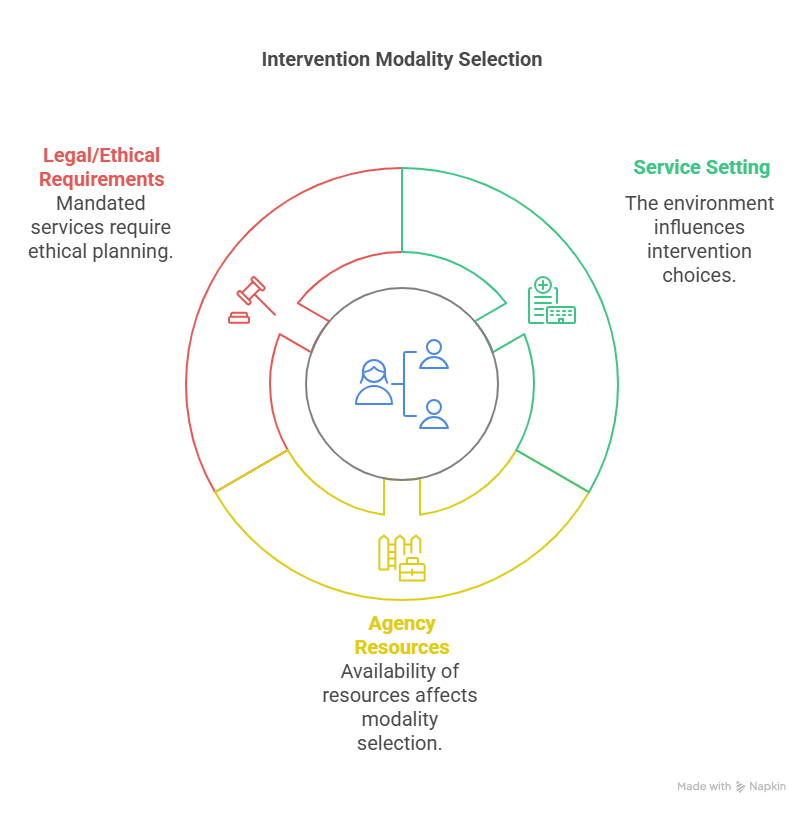
Accessible Image Description:
Contextual and Systemic Considerations:
-
Service Setting: School, private practice, hospital, community center, etc., will impact the type of intervention/treatment options.
-
Agency Resources or Constraints: Access to certain modalities may be limited by training, insurance, or policy.
-
Legal or Ethical Requirements: In mandated services, options may be restricted. However, treatment planning still requires ethical planning, even if the client is mandated.
the components of intervention, treatment, and service plans
Components that should be included in a treatment plan (also referred to as a service plan, contract, etc.):
- Identified problem
- Goals
- Objectives (also referred to as action steps)
- Intervention strategies
- Timeline
- Roles and responsibilities
- Evaluation method
- Client strengths and resources
- Client participation and agreement
| Component | Description |
|---|---|
| Identified Problem(s) | Clearly stated, client-centered issues based on the assessment process |
| Goals | Broad, long-term desired outcomes (e.g., “Improve emotional regulation”) |
| Objectives | Specific, measurable, time-limited steps toward goals (e.g., “Use coping skills in 3 of 4 stressful situations per week”) |
| Intervention Strategies | Specific methods or actions the social worker and client will take (e.g., CBT sessions, referrals) |
| Timeline | Time frame for achieving goals and reviewing progress (e.g., 3-month plan with biweekly sessions) |
| Roles and Responsibilities | Defined tasks for client, social worker, and any involved systems (e.g., case manager, school counselor) |
| Evaluation Method | Plan for monitoring progress and evaluating outcomes (e.g., self-report, attendance, mood scales) |
| Client Strengths and Resources | Incorporate personal and environmental strengths to support goals |
| Client Participation/Agreement | Client must understand and agree to the plan; signatures often required in formal settings |
Self-Check
psychotherapies
In a prior section in this chapter, there is a table with several modalities and brief highlights on when the modalities might be used. The Masters exam does not expect detailed implementation knowledge about psychotherapies.
Exam Information to Keep In Mind
A social worker should be able to:
-
Identify the appropriate modality during intervention planning (focus on studying common interventions).
-
Recognize when referral to a specialist in a particular psychotherapy is needed.
Think of psychotherapy on the exam as part of matching the right tool to the right person in the right setting. Know what the main types are, what they are used for, and how to choose them collaboratively and ethically.
Self-Check
The following question set includes eight recall questions about psychotherapy modalities. After answering a question, click on the ‘check’ icon.
the impact of immigration, refugee, or undocumented status on service delivery
Immigration status, whether documented, refugee, asylum-seeking, or undocumented, can profoundly affect a client’s access to services, sense of safety, and willingness to engage with social systems.
Exam Information to Keep In Mind
-
Prioritize safety, trust-building, and client autonomy.
-
Use trauma-informed, strengths-based approaches that validate the client’s experience.
-
Connect clients to immigration legal services, culturally specific community supports, and interpreter services when needed.
Key Considerations:
1. Access to Services:
- Undocumented clients may avoid seeking help due to fear of deportation or lack of insurance.
-
Refugees and asylum seekers may face language barriers, housing insecurity, or difficulty navigating unfamiliar systems.
-
Legal status often determines access to public benefits, mental health services, housing, and employment support.
2. Trauma and Loss:
-
Some immigrant and refugee clients have experienced displacement, persecution, violence, family separation, or trauma during migration.
-
Even the legal process for immigration can involve loss of identity, status, community, and support systems.
3. Cultural and Language Barriers:
-
Mistrust of government systems and mental health stigma may lead to resistance or disengagement.
-
Interpretation services and culturally congruent care are essential for ethical service delivery.
4. Ethical and Legal Responsibilities:
-
Social workers must never disclose immigration status without consent.
-
Understand mandated reporting laws but avoid overreporting based on cultural misunderstandings.
-
Advocate for client rights and access to services regardless of immigration status.
discharge, aftercare, and follow-up planning
Termination can be viewed as an umbrella term; the overall process of ending the professional relationship between the social worker and the client. Termination includes both the ethical and procedural responsibilities that come with ending services.
Note: Discharge, aftercare, and follow-up are words that are sometimes used interchangeably. However, there are some differences.
Discharge is the formal conclusion of services with a client. Discharge marks the end of the social worker-client relationship and should include a summary of progress, services provided, outstanding needs, risk level, and the reason for ending services.
-
Focus: Closure of the formal intervention
-
Timing: Happens at the end of treatment or services
-
Example: “The client met their goals and is being discharged from outpatient care.”
Quick Breakdown
Discharge Planning Begins Early
-
Discharge planning is a proactive process.
-
Should be discussed early in treatment and revisited regularly as progress is made.
Indicators for Discharge Readiness
-
Client has met treatment goals
-
Client expresses a desire to end services
-
Client is consistently stable and self-sufficient
-
No further need for ongoing support at the current level of care
Aftercare refers to the support plan developed for the client to maintain progress after discharge. Aftercare involves referrals, resources, and recommendations that help the client continue care or navigate challenges independently.
-
Focus: Sustaining progress post-discharge
-
Timing: Planned before discharge, carried out after
-
Example: “The aftercare plan includes weekly support group meetings and a referral to a housing agency.”
Quick Breakdown
Barriers to Aftercare
-
Clients may face:
-
Transportation issues
-
Language barriers
-
Lack of insurance or eligibility
- Employment barriers (e.g., limited benefits like sick leave to go to appointments)
-
-
Social workers should anticipate and problem-solve these barriers during the discharge planning process.
Follow-up involves checking in with the client after discharge to monitor well-being, offer support, or ensure connection to services. Follow-up may be one-time or ongoing, depending on agency policy and service delivery.
-
Focus: Reassessment or reconnection after discharge
-
Timing: Occurs after discharge as a post-service contact
-
Example: “The social worker followed up 30 days after discharge to confirm the client accessed their new therapist.”
Exam Information to Consider
Setting: Keep in mind the setting of the social worker. A hospital discharge plan might include referrals to outpatient physical therapy, case management, or primary care. In a school, this process may involve coordination with parents or IEP support. Think about how context shapes the termination process.
Client-Centered: The best answers are usually those that prioritize the client’s voice, goals, and readiness in the discharge planning process. Even if services are ending, the client should still be involved in planning the next steps.
Consider Risk: If the client has safety risks or concerns (e.g., suicidal ideation, domestic violence, unstable housing), discharge should include a clear risk management or safety plan. This is an important intervention planning process to ensure safety and support.
Documentation: The discharge note should include details about progress, risk, client input, and continuity of care.
Techniques used for follow-up
| Technique | Description |
|---|---|
| Scheduled Check-Ins | Pre-arranged phone calls, emails, or meetings to assess client well-being and progress. |
| Home Visits | In-person follow-up to observe living conditions and ensure safety, especially in child welfare or housing cases. |
| Progress Monitoring Tools | Use of checklists, goal reviews, or self-report assessments to measure continued progress or setbacks. |
| Coordination with Providers | Contacting service providers (with consent) to verify attendance, progress, or challenges with referrals or interventions. |
| Booster Sessions | Brief, periodic follow-up sessions to reinforce skills, problem-solve challenges, or provide motivation. |
| Crisis Planning Review | Revisiting or updating safety/crisis plans to ensure clients are prepared for future stressors or risks. |
| Referrals and Re-Linking | Providing new or additional referrals if needs have changed or previous services were not sustained. |
| Follow-Up Letters/Notes | Written communication reminding clients of resources, supports, or upcoming appointments. |
Self-Check
The following activity is a question set. After answering a question, click on the ‘check’ icon.
The indicators of client/client system readiness for termination
The NASW Code of Ethics 1.17 highlights information about the termination of services.
NASW Code of Ethics 1.17: Termination of Services
- “(a) Social workers should terminate services to clients and professional relationships with them when such services and relationships are no longer required or no longer serve the clients’ needs or interests.
- (b) Social workers should take reasonable steps to avoid abandoning clients who are still in need of services. Social workers should withdraw services precipitously only under unusual circumstances, giving careful consideration to all factors in the situation and taking care to minimize possible adverse effects. Social workers should assist in making appropriate arrangements for continuation of services when necessary.
- (c) Social workers in fee-for-service settings may terminate services to clients who are not paying an overdue balance if the financial contractual arrangements have been made clear to the client, if the client does not pose an imminent danger to self or others, and if the clinical and other consequences of the current nonpayment have been addressed and discussed with the client.
- (d) Social workers should not terminate services to pursue a social, financial, or sexual relationship with a client.
- (e) Social workers who anticipate the termination or interruption of services to clients should notify clients promptly and seek the transfer, referral, or continuation of services in relation to the clients’ needs and preferences.
- (f) Social workers who are leaving an employment setting should inform clients of appropriate options for the continuation of services and of the benefits and risks of the options” (Source: NASW Code of Ethics).
Key Indicators: The client should take an active role in discussing goal attainment with the social worker (remember collaboration when answering termination questions) based on the client’s treatment plan. When a client has reached their goals in their treatment plan, this is a key indicator of readiness for termination. Goal attainment is not ‘perfection’ and can include a client gaining insights into their experiences, the ability to regulate their emotions, and the ability to recognize coping skills that enhance their wellness. Termination is a process, and social workers should always keep termination in mind. The importance of the strengths perspective cannot be overstated.
Additional indicators:
- Client expresses a desire to end services.
- Client’s well-being is improved.
- No further need for ongoing support at the current level of care
Exam Information to Consider
- Keep in mind the NASW Code of Ethics 1.17.
- Watch for any termination questions on the exam that do not honor the right to self-determination and/or collaboration.
- Examine the role of the social worker. Even if a social worker only works with a client once or twice, termination is still an important process.

