28 Impact of Trauma and Trauma-Informed Care
Alexandria Lewis
Content Outline, Competency, and KSAs
I. Human Development, Diversity, and Behavior in the Environment
1A. Human Growth and Development
KSAs:
– The impact of stress, trauma, and violence
– Theories of trauma-informed care
II. Assessment and Intervention Planning
IIA. Biopsychosocial History and Collateral Data
KSAs:
– Methods used to assess trauma
– The indicators of traumatic stress and violence
III. Interventions with Clients/Client Systems
IIIA. Intervention Processes and Techniques or Use Across Systems
– Methods and approaches to trauma-informed care
overview
Definitions:
- Trauma:
- “any disturbing experience that results in significant fear, helplessness, dissociation, confusion, or other disruptive feelings intense enough to have a long-lasting negative effect on a person’s attitudes, behavior, and other aspects of functioning. Traumatic events include those caused by human behavior (e.g., rape, war, industrial accidents) as well as by nature (e.g., earthquakes) and often challenge an individual’s view of the world as a just, safe, and predictable place” (APA Dictionary).
- “Individual trauma results from an event, series of events, or set of circumstances that is experienced by an individual as physically or emotionally harmful or life threatening and that has lasting adverse effects on the individual’s functioning and mental, physical, social, emotional, or spiritual well-being” (The Substance Abuse and Mental Health Services Administration [SAMHSA]).
- Stress:
- “the physiological or psychological response to internal or external stressors. Stress involves changes affecting nearly every system of the body, influencing how people feel and behave. For example, it may be manifested by palpitations, sweating, dry mouth, shortness of breath, fidgeting, accelerated speech, augmentation of negative emotions (if already being experienced), and longer duration of stress fatigue” (APA Dictionary).
Trauma
Trauma and the Brain
Trauma can impact the brain:
- Rewiring of the brain.
- Emotion networks, resulting in under or over-reacting to stressful situation.
- Affects the amygdala, hippocampus, and prefrontal context.
Three Ways Trauma Can Change the Brain
Polyvagal Theory and How Trauma Impacts the Brain
How Trauma Impacts Four Different Types of Memory
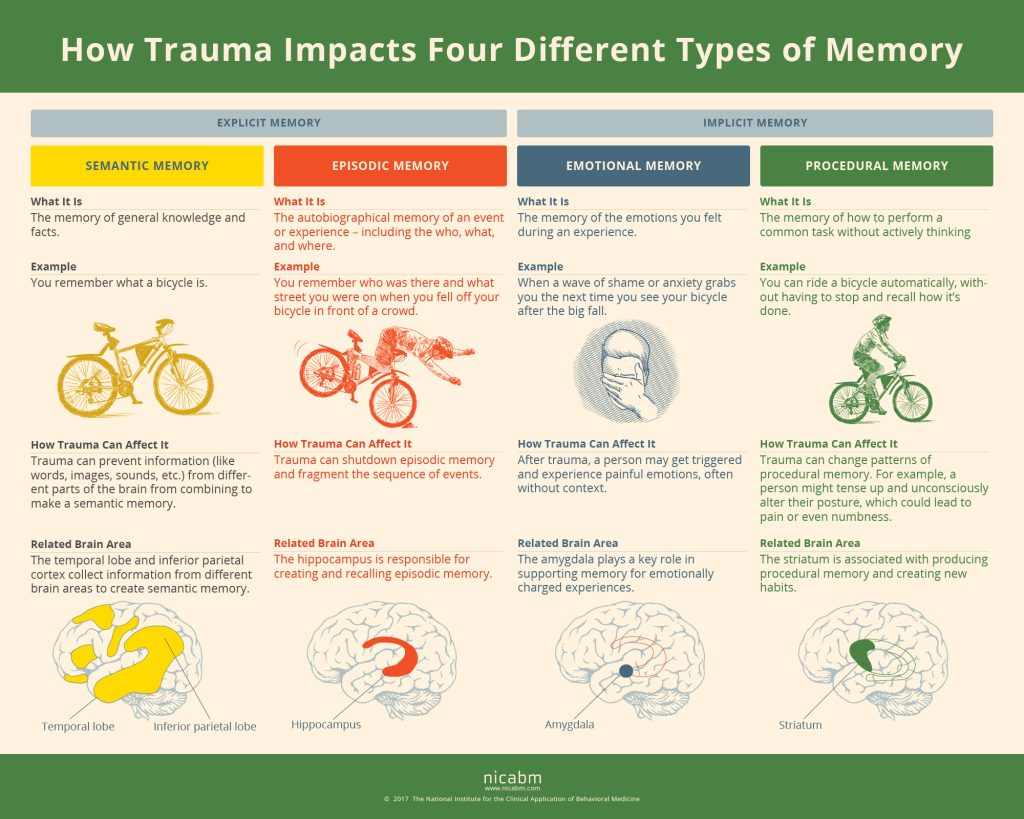
Text-Only Version of the Infographic (Source: NICABM)
How Trauma Impacts the Four Different Types of Memory
Explicit Memory:
- Semantic Memory:
- How Trauma Can Affect It: Trauma can prevent information (like words, images, sounds, etc.) from different parts of the brain from combining to make a semantic memory.
- Related Brain Area: The temporal lobe and inferior parietal cortex collect information from different brain areas to create semantic memory.
- Episodic Memory:
- How Trauma Can Affect It: Trauma can shutdown episodic memory and fragment the sequence of events
- Related Brain Area: The hippocampus is responsible for creating and recalling episodic memory.
Implicit Memory:
- Procedural Memory:
- How Trauma Can Affect It: Trauma can change patterns of procedural memory for example, a person might tense up and unconsciously alter their posture, which could lead to pain or even numbness.
- Related Brain Area: The striatum is associated with producing procedural memory and creating new habits.
- Emotional Memory:
- How Trauma Can Affect It: After trauma, a person may get triggered and experience painful emotions, often without context.
- Related Brain Area: The amygdala plays a key role in supporting memory for emotionally charged experiences.
How the Nervous System Responds to Trauma
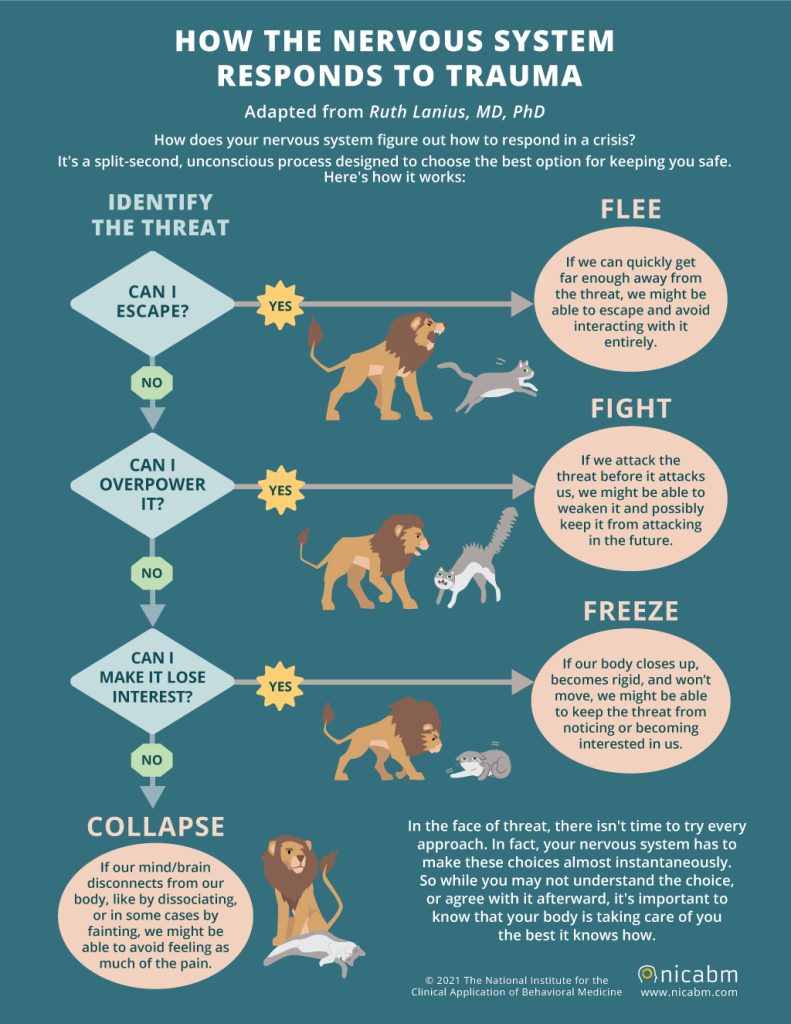
Text-Only Version of the Infographic (Source: NICABM)
How does your nervous system figure out how to respond in a crisis?
It’s a split- second, unconscious process designed to choose the best option for keeping you safe. Here’s how it works.
Identify the Threat. Can I escape?
If yes, then flee. If we can quickly get far enough away from the threat, we might be able to escape and avoid interacting with it entirely.
If I can’t escape, can I overpower it?
If yes, then fight. If we attack the threat before it attacks us, we might be able to weaken it and possibly keep it from attacking in the future.
If I can’t overpower it, can I make it lose interest?
If yes, then freeze. If our body closes up, becomes rigid, and won’t move, we might be able to keep the threat from noticing or becoming interested in us.
If I can’t make it lose interest, then collapse. If our mind/brain disconnects from our body, like by dissociating, or in some cases by fainting, we might be able to avoid feeling as much of the pain.
In the face of threat, there isn’t time to try every approach. In fact, your nervous system has to make these choices almost instantaneously. So while you may not understand the choice, or agree with it afterward, it’s important to know that your body is taking care of you the best it knows how.
Impact of stress
Stress can impact body systems, including reproductive systems, cardiovascular, endocrine, gastrointestinal, respiratory, and musculoskeletal. The following is a reader-friendly resource highlighting how stress can impact systems of the body: Stress Effects on the Body (APA).
Stress in Childhood
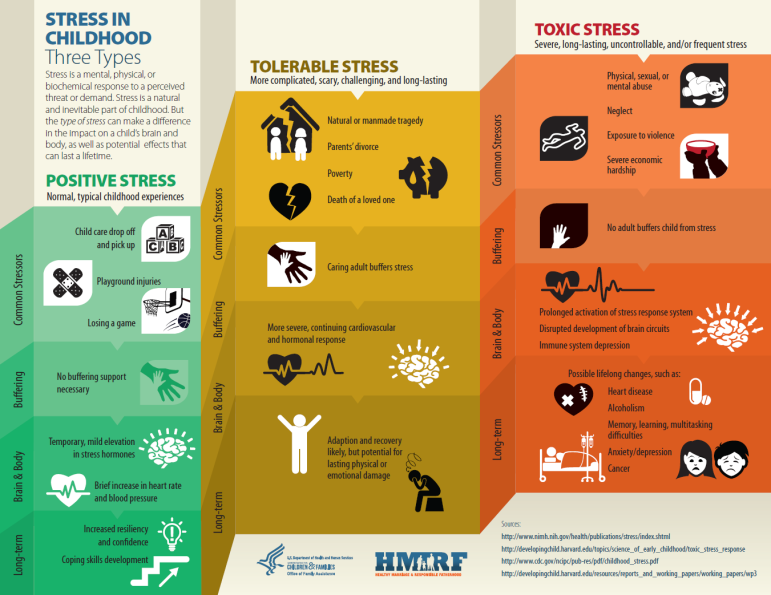
Video: Toxic Stress and the Brain
Video: Understanding Adverse Childhood Experiences (ACEs)
Resources:
- What is Toxic Stress (handout)
- ACEs Aware website
- ACEs and Toxic Stress Infographic
- ACEs Infographic (CDC)
methods used to assess trauma
The following are examples of methods that can be used to assess trauma.
- Clinical Interviews and Assessment Tools: Structured or semi-structured interviews that allow clinicians to gather in-depth information about an individual’s trauma history, symptoms, and the impact of trauma on their functioning.
- Trauma and Stressor Exposure Measure Examples (National Center for PTSD): Brief Trauma Questionnaire, Life Events Checklist for DSM 5, Life Stressor Checklist, Trauma Assessment for Adults, Trauma History Questionnaire, and Trauma History Screen.
- Observational Methods: Observations of behavior, mood, and interactions can provide valuable insights into the effects of trauma on an individual. This can be particularly useful in settings where individuals may not be able to articulate their experiences directly, such as with young children or those with significant communication barriers.
- Biological and Physiological Assessments: In some cases, assessments may include the examination of biological or physiological responses to stress or reminders of trauma. This can involve measures of heart rate, cortisol levels, or brain imaging studies to identify areas of the brain affected by trauma.
- Ecological or Contextual Assessments: Assessing the individual’s environment and social context to understand the impact of trauma. This includes evaluating safety, support systems, and ongoing stressors that may influence trauma recovery.
- Cultural and Sociodemographic Considerations: Understanding the cultural background and sociodemographic factors that can influence an individual’s experience and expression of trauma. This includes being aware of cultural norms, stigma associated with trauma, and access to resources.
- Functional Assessments: Evaluating how trauma affects an individual’s daily functioning across various domains such as work, school, relationships, and self-care. This helps in identifying specific areas where the individual may need support or intervention.
These methods should not be used as isolated within a vacuum and using more than one method provides a comprehensive understanding of an individual’s trauma experiences. It is important to consider the client’s age, the nature of the trauma, cultural factors, and the specific symptoms or issues presented.
Trauma Informed care
The SAMHSA defines Trauma-Informed Care (TIC) as a framework that involves understanding, recognizing, and responding to the effects of all types of trauma. TIC emphasizes physical, psychological, and emotional safety for both clients/patients and providers, and helps survivors rebuild a sense of control and empowerment.
The SAMHSA identifies six key principles of a trauma-informed approach:
1. Safety
2. Trustworthiness and Transparency
3. Peer support
4. Collaboration and mutuality
5. Empowerment, voice, and choice
6. Cultural, historical, and gender Issues
TIC acknowledges the need to understand a patient’s life experiences in order to deliver effective care. It has the potential to improve patient engagement, treatment adherence, health outcomes, and provider and staff wellness.
The Center for Health Care Strategies, Inc, highlighted the following key ingredients for creating a trauma-informed approach to care:
- Organizational:
- Engaging patients in organizational planning.
- Creating a safe environment.
- Preventing secondary traumatic stress among staff.
- Providing trauma-informed training to all staff.
- Clinical:
- Collaborating with clients in the treatment process.
- Assessing for trauma.
- Utilizing trauma-specific treatment and training staff.
Source: Issue Brief- Key Ingredients for Successful Trauma-Informed Care Implementation
Resource:
self check

