7 Case Analysis 2: Mr. Stancil’s Sticky Situation
Learning Objectives
Process Learning Objectives:
Through authentic practice and shared inquiry in this case, students will develop:
- Information literacy skills, including the ability to locate, access, evaluate and use information in a wide range of situations.
- Awareness of the role of emotions in learning.
- Self-directed learning and metacognitive strategies to maximize their learning effectiveness.
- Fluency in reading, writing, summarizing, speaking, listening, viewing and presenting information.
- Social skills critical to effective team functioning, including interacting, cooperating, collaborating, and mutual respect for others’ ideas.
Content Learning Objectives:
Through authentic practice and shared inquiry in this case, students will develop a deep understanding of cardiovascular disease including:
- Etiology, symptoms and causes of thrombosis and atherosclerosis
- Diagnosis and classification of thrombosis and atherosclerosis
- Diagnostic features of DVT on venous doppler sonography
- Diagnostic features of positive V/Q scans
- Diagnostic features of stroke on head CT
- Management and treatment of thrombosis and atherosclerosis
- Prevention of thrombosis and atherosclerosis
- Outlook/Prognosis for those with thrombosis and atherosclerosis
- Common comorbidities of thrombosis and atherosclerosis
The Case of Mr. Stancil’s Sticky Situation
Mr. Stancil, a 58 Y/O male, arrives at the Emergency Room complaining of left leg pain. He reports that his left leg pain started last week after driving a tractor 14 hours /day for 5 days. He treated the pain with Acetaminophen, but experienced minimal relief. The pain increased significantly after a 750 mile car trip to his son’s house yesterday. Upon rising this morning, he reports that his left leg was swollen and painful, that his chest hurt, and that he had shortness of breath. He also reports that his Coumadin prescription did not come in the mail before he left home, so he hasn’t taken it in “a couple of days.”
History and Assessment
|
Past Medical History
|
|
Social and Family History Family history is negative for ischemic heart disease. Mr. Stancil’s mother had adult onset diabetes. His father died at age 93. Mr. Stancil does not drink, and has reduced his cigarette smoking to ½ pack per day since his heart surgery. (He previously smoked 1 pack per day for 50 years.) He is self-employed as a farmer.
|
Immediate Assessment
- Height: 173 cm
- Weight: 110 kg
- B.P.: 155/95 mmHg
- Pulse: 110 b/min
- Respiration rate: 20 b/min
- Temperature: 38.2 ºC
- SpO2: 87%
Mr. Stancil is alert and oriented X3, in mild distress. He has 2+ pitting edema of the left leg with erythema that is warm to the touch. He has a positive Homan’s sign on the left leg, negative on the right leg. He has positive calf pain on the left; pain increases with standing and walking.
Dr. Murphy, the emergency room attending physician has performed an initial assessment. An IV with a normal saline drip is started. Mr. Stancil is also supplied with 4 L/min oxygen by nasal cannula. Dr. Murphy orders a Hematology Profile (HP), blood chemistries, coagulation panel and D-dimer.
Lab Results
| Result | Normal Range | |
| Hematology Profile:
Leukocyte count (WBC) |
10.1 |
4.5-11 (103/mm3) |
| Erythrocyte count (RBC) | 4.5 | 4.5-5.3 (103/mm3) |
| Hemoglobin | 14 | 13.5-18 g/dl |
| Hematocrit | 42 | 40-54% |
| Platelet | 164 | 150-400 K/ul |
| D-dimer | 0.550 | <0.5 mcg/mL |
| Coagulation Panel:
PT |
14 |
11.7-14.5 seconds |
| PTT | 30 s | 22.6-32.9 seconds |
| Chemistries:
Creatinine |
1.5 |
0.8-1.5 g/dl |
| BUN | 25 | 12-25 g/dl |
Dr. Murphy is concerned with the high D-dimer and orders a STAT portable CXR and bilateral lower extremity ultrasound.
Stop here!
Identify important observations and generate hypotheses based on your observations. Using numbers or arrows (or some other system), link each hypothesis to the observation(s) which support that hypothesis. What assessments/interventions should occur next in Mr. Stancils’s care?
Begin your list of learning issues.
The radiologic technologist arrives and completes Mr. Stancil’s portable CXR.

Radiology Report
Examination: AP Chest
History: Shortness of breath and chest pain.
Findings: An upright AP chest x-ray was obtained. Heart size is within the normal range.
Impression: Normal chest x-ray.
Radiology Report
Examination: Duplex Lower Extremity Veins, Bilateral
History: Left leg swelling and pain
Findings: Real-time Doppler ultrasound of both lower extremities was performed.
Right lower extremity: No evidence of thrombus is seen in the common femoral, superficial femoral or popliteal veins. The veins show good compressibility and augmentation of flow.
Left lower extremity: An intraluminal filling defect is seen in the left femoral vein just distal to the confluence of the left femoral and profunda veins. The caudal end of the filling defect extends to the level of the popliteal vein.
Impression:
Negative exam for DVT in right lower extremity.
Positive exam for DVT in left femoral and popliteal veins
Stop here!
Identify important observations and generate hypotheses based on your observations. Using numbers or arrows (or some other system), link each hypothesis to the observation(s) which support that hypothesis. What assessments/interventions should occur next in Mr. Stancil’s care?
Add to your list of learning issues.
Mr. Stancil is alert and oriented, complaining of shortness of breath and chest pain. Auscultation reveals crackles. There is an increased systolic murmur over the left sternal border that is louder during inspiration.
Dr. Murphy places Mr. Stancil on 4L/min O2 by nasal cannula and orders Arterial blood gasses, a STAT ECG and a V/Q scan. The respiratory therapist draws the ABGs and sends the sample to the lab.
| Result | Normal Range | |
| Arterial Blood Gas:
pH |
7.49 H |
7.35-7.45 |
| PaCO2 | 30 L |
35-45 (mmHg) |
| PaO2 | 55 L |
>100 (mmHg) |
| SaO2 | 89 L |
>95 (%) |
| HCO3- | 27 H |
22-26 (mEq/L) |
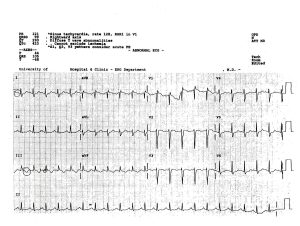
The ECG was interpreted as Abnormal, 3eith sinus tachycardia, rate 128; R5R1 in V1 Rightward axis; Diffuse T wave abnormalities. Cannot exclude ischemia. S1, Q3, T3 pattern consider acute PE.
Stop here!
Identify important observations and generate hypotheses based on your observations. Using numbers or arrows (or some other system), link each hypothesis to the observation(s) which support that hypothesis. What assessments/interventions should occur next in Mr. Stancil’s care?
Add to your list of learning issues.
Mr. Stancil is transported to Nuclear Medicine for the V/Q scan.
Nuclear Medicine Report
Examination: Ventilation/Perfusion Scan
Radioaerosol Image: A standard xenon ventilation study with wash-in, equilibrium and washout was performed. Results within normal range.
Lung Perfusion: 5 mCi of Tc-99m MAA were injected AC (antecubital) as the patient lay supine with normal breathing. Anterior, posterior, both laterals, and both posterior oblique projections were acquired. Multiple segmental mismatched defects are noted in the lower lungs bilaterally and in the right lung.
Findings: The probability for bilateral multiple PE is high. Recommend immediate pulmonary angiography.

Mr. Stancil is taken from Nuclear Medicine to Interventional Radiology for a Pulmonary Angiogram.
Radiology Report
Examination: Pulmonary Angiogram
History: Multiple segmental mismatched defects on V/Q scan
Procedure: Using aseptic conditions under fluoroscopic monitoring and guidance, the right common femoral vein was catheterized via an anterior wall puncture. A preformed 7 French pigtail catheter was advanced to the left pulmonary artery in antegrade fashion without complications. Pulmonary pressure was measured. Injection of iso-osmolar water-soluble contrast medium was then followed by digital subtraction imaging of the thorax in the RAO projection.
Findings: Pulmonary pressure measured 52/32 with a mean of 38 mm Hg. There is evidence of bilateral pulmonary emboli. A saddle embolus on the right extends into the truncus anterior and the inferior division of the pulmonary artery and is occluding branches to the right upper and lower lobes. Additional emboli are seen in the left lower lobe.
Impression: Bilateral pulmonary emboli with massive acute right and significant left pulmonary emboli. Recommend STAT transcatheter therapy.
Intervention: Transcatheter therapy with Urokinase is initiated via the right femoral vein. The Urokinase infusion will continue throughout the night for a total infusion of 150,000 units. An inferior vena cava filter is considered but deferred at this time.
0800 Mr. Stancil returns to Interventional Radiology for evaluation of the effectiveness of the transcatheter therapy under fluoroscopy. Visipaque 320 is injected and images obtained. Images show marked improvement of the peripheral circulation within the lungs as well as dissolution of a significant amount of the clot seen centrally in the pulmonary artery. Overall perfusion in both the right and left lungs has improved. The patient’s oxygenation by ABG shows marked improvement. Urokinase is decreased to 10,000 units per hour and heparin is added at 700 units per hour. The patient is scheduled to return at 16:00.
1600 The patient returns to Interventional Radiology. Visipaque 320 is injected and images obtained. Peripheral circulation is good and the central pulmonary artery clot has been resolved. The UK infusion is stopped and the catheter removed.
Discharge: Mr. Stancil is given a prescription for Coumadin. He is counseled on the proper use of the drug and the importance of proper diet and exercise.
Stop here!
Identify important observations and generate hypotheses based on your observations. Using numbers or arrows (or some other system), link each hypothesis to the observation(s) which support that hypothesis. What assessments/interventions should occur next in Mr. Stancil’s care?
Add to your list of learning issues.
Four Months Later…
Mr. Stancil presents to a small community hospital ED via private vehicle. Patient complains of nausea, vomiting, and HA (headache) that radiates to his back.
Family reports that Mr. Stancil has had 3-4 days of left sided HA, which he has treated unsuccessfully with OTC pain relievers. They report the onset of more severe pain this morning, and even tried applying ice packs to his head. About noon today his left-sided HA continued to worsen and he also began to complain of back pain. The family attempted giving a backrub, without significant improvement. Mr. Stancil tried lying on the floor to stretch his back. He then began to vomit. He finally agreed to go to the ED after the vomiting began, but refused to allow his family to call an ambulance. He was driven to the ED by family members. He continued to vomit en route to the ED and he began to have some difficulty speaking.
The family denies any previous or recent trauma to his head. They report that he has never had any episodes like this and that his past medical history is significant for CAD, DVT, and PE.
Radiology Report
Examination: non-contrast Head CT
History: Left-sided headache
Findings: Positive for a midline shift and obliteration of the right ventricle, consistent with hemorrhagic stroke.
Impression: There is a large left sub-dural hematoma (SDH) as well as a left-sided sub-arachnoid hemorrhage (SAH). The SDH has resulted in a left-to-right midline shift which includes the brain stem.
Media Attributions
- Stancil’s Chest X-ray
- Stancil EKG
- Article Frontiers docx

