6 Case Analysis 1: Ms. Montoya’s BIG Problem
Learning Objectives
Process Learning Objectives:
Through authentic practice and shared inquiry in this case, students will develop:
- Information literacy skills, including the ability to locate, access, evaluate and use information in a wide range of situations.
- Awareness of the role of emotions in learning.
- Self-directed learning and metacognitive strategies to maximize their learning effectiveness.
- Fluency in reading, writing, summarizing, speaking, listening, viewing and presenting information.
- Social skills critical to effective team functioning, including interacting, cooperating, collaborating, and mutual respect for others’ ideas.
Content Learning Objectives:
Through authentic practice and shared inquiry in this case, students will develop a deep understanding of obesity including:
- Etiology, symptoms and causes of obesity
- Diagnosis and classification of obesity
- Management and treatment of obesity
- Prevention of obesity
- Outlook/Prognosis for those with obesity
- Common comorbidities of obesity
The Case of Ms. Montoya
Ms. Montoya is a 46-year old Hispanic woman, who was recently diagnosed with severe obstructive sleep apnea with oxygen desaturations to 82%. She is being treated with a Bi-PAP at 21/17cm of water pressure with heated humidifier.
History and Assessment
|
Past Medical History
|
|
Family History Mrs. Montoya is married, with 2 children, ages 26 and 19. She recently started working full-time for an insurance company doing data entry and other clerical work, because her grandson started school. Neither she nor her husband smoke.
|
Immediate Assessment
- Ht 5’10”
- Wt 416#
- BP 154/94 mmHg
- Pulse 108/min
- Respiratory rate 23/min
Current Medications
- Lexapro 10 mg, once daily
- Captopril 25 mg, 3 times daily
- Toprol 25 mg, once daily
- Albuterol inhaler, as needed
- Lipitor 20 mg, once daily
- Metformin IR 850 mg, twice daily
Dr. Oscar, Ms. Montoya’s primary care physician, has referred Ms. Montoya to Dr. Wheeler for a bariatric evaluation. Ms. Montoya has attended the introductory seminar and returned the medical questionnaire as requested. Copies of lab results have been received.
Lab Results – Metabolic Panel
|
Test |
Result |
H/L |
Ref Range Low |
Ref Range High |
UOM |
|
Glucose |
140 |
H |
57.0 |
110.0 |
mg/dL |
|
BUN |
10 |
|
8.0 |
23.0 |
mg/dL |
|
Creat |
0.6 |
L |
0.7 |
1.6 |
mg/dL |
|
Na |
134 |
|
134 |
145 |
mmol/L |
|
K |
3.8 |
|
3.4 |
5.3 |
mmol/L |
|
Cl |
100.7 |
L |
101 |
113 |
mmol/L |
|
Calcium |
9.0 |
|
8.4 |
10.2 |
mg/dL |
|
Alk Phos |
46 |
|
20.0 |
108.0 |
IU/L |
|
CO2 |
25.0 |
|
23.0 |
33.0 |
mmol/L |
|
AST |
54 |
H |
10.0 |
42.0 |
IU/L |
|
ALT |
38 |
|
10.0 |
60.0 |
IU/L |
|
TL Prot |
6.7 |
|
6.3 |
7.7 |
Gm/DL |
|
Albumin |
4.0 |
|
3.5 |
5.0 |
Gm/DL |
|
TBili |
0.9 |
|
0.1 |
1.3 |
mg/dL |
|
OSMO |
269.6 |
|
269.0 |
302.0 |
MOSM/L |
|
Anion Gap |
12.1 |
|
0.0 |
26.0 |
|
|
BUN/Cre |
16.7 |
|
10.0 |
20.0 |
|
|
Chol |
400 |
H |
130 |
240 |
mg/dL |
|
Trigl |
600 |
H |
30 |
150 |
mg/dL |
Dr. Wheeler advises Ms. Montoya that he believes she has metabolic syndrome. He recommends bariatric surgery due to her comorbidities in addition to her body mass index. He asks her to decide whether she wishes to pursue the Laparoscopic Adjustable Gastric Band procedure or the Laparoscopic Roux en Y Divided Gastric Bypass procedure.
Stop here!
Identify important observations and generate hypotheses based on your observations. Using numbers or arrows (or some other system), link each hypothesis to the observation(s) which support that hypothesis. What assessments/interventions should occur next in Ms. Montoya’s care?
Begin your list of learning issues.
After some thought and discussion with her husband and daughter, Ms. Montoya has elected to undergo the Roux en Y procedure. She has been scheduled for pre-op labs, CXR and an anesthesiology consult the evening prior to her surgery. She arrives at admissions and, after completing the required paperwork, is taken to radiology and lab before being taken to her room.
Radiology Report
Examination: PA and Lat Chest
History: Pre-op
Findings: PA and lateral views of the chest reveal satisfactory inspiration with no evidence of active cardiopulmonary disease. The cardiac silhouette is normal in size and configuration and the visualized osseous structures are unremarkable.
Impression: Normal PA and lateral chest.
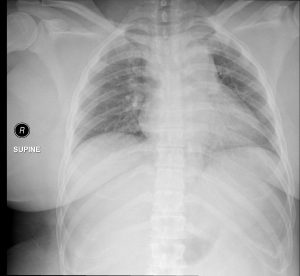

Case courtesy of Andrew Dixon, Radiopaedia.org, rID: 31644
Lab Results
Adm Diag:Pre Op
|
Test |
Result |
H/L |
Ref Range Low |
Ref Range High |
UOM |
|
PT |
12.7 |
|
10.1 |
13.9 |
Sec |
|
Fibrinogen |
1.1 |
|
0 |
4.1 |
g/L |
|
APTT |
25.5 |
|
19.8 |
30.2 |
sec |
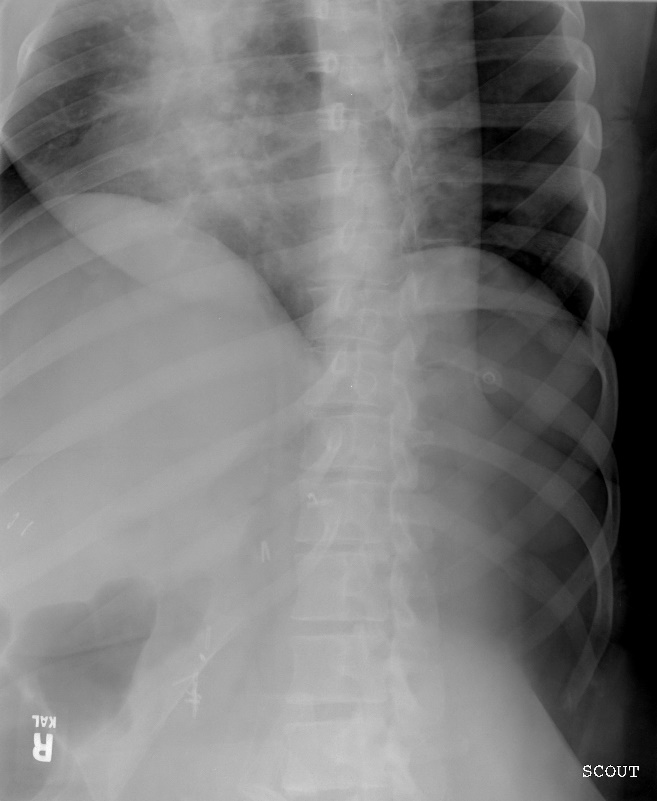
Later that night, once she is settled into her room, Ms. Montoya records her thoughts on the day…
Stop here!
Identify important observations and generate hypotheses based on your observations. Using numbers or arrows (or some other system), link each hypothesis to the observation(s) which support that hypothesis. What assessments/interventions should occur next in Ms. Montoya’s care?
Add to your list of learning issues.
The next morning, Ms. Montoya is taken to surgery. The laproscopic Roux en Y procedure is successfully performed, creating a 15 cc pouch. No air leak is noted intraoperatively. A penrose drain is placed at the G-J anastomosis. After recovering from anesthesia, she is taken back to her room.
The next morning, Dr. Wheeler stops in to check on Ms. Montoya, and the nurse records her vital signs.
Progress NotesPatient is without complaints. Has been walking. Pain needs better control. No CPAP on, but no shortness of breath.
Vitals: T- 37.9; P – 82; BP – 136/88; R – 24; SpO2 – 93-97% NC4L
Labs: Hgb/Hct stable. ABGs OK.
Physical Exam: No abdominal distention (NAD). Pt. is alert and oriented x3 (A&Ox3), in some pain. Regular heart rate and rhythm (RRR). Lungs are clear bilaterally. Abdomen is soft, nondistended, tender to palpation in the Left upper quadrant. L penrose has serous drainage.
Orders: 46 yof s/p LRYGB POD#1
- UGI and methyl blue today
- Better control of pain
- Continue bariatric protocol
After administering some pain meds, Ms. Montoya is feeling better and is able to move without pain. She is sent to Radiology for the Upper GI study.
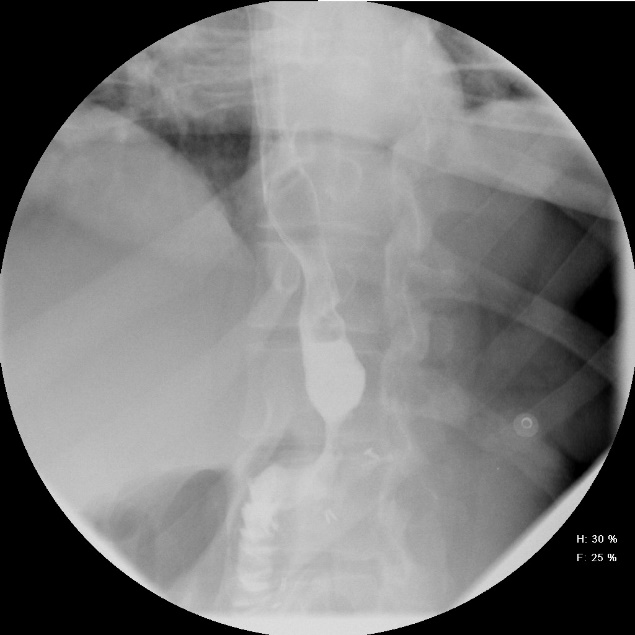
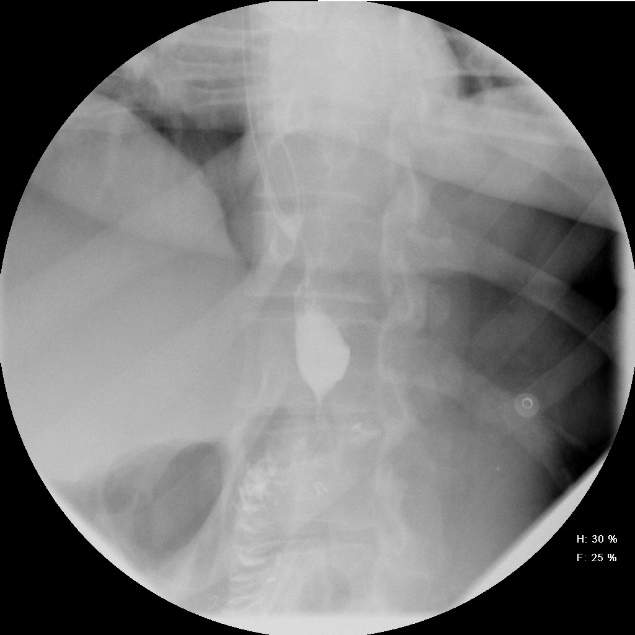
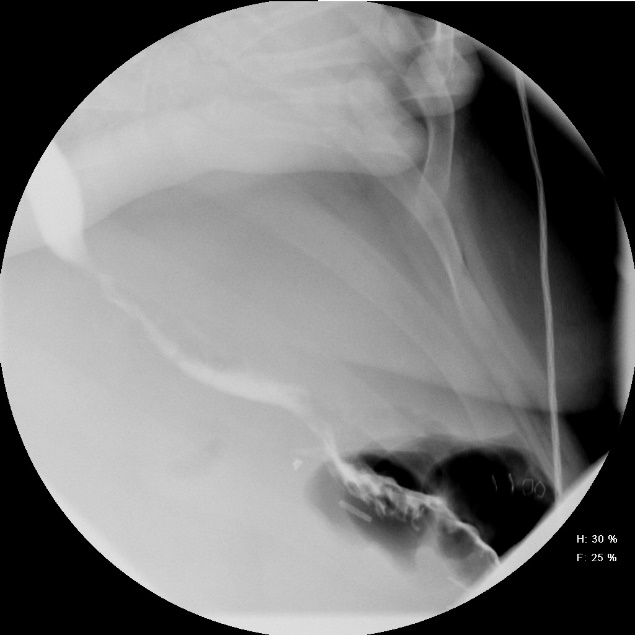
Radiology Report
Examination: Post-op Bariatric UGI
History: 46 yof s/p LRYGB POD#1
Findings: No site of leak or obstruction.
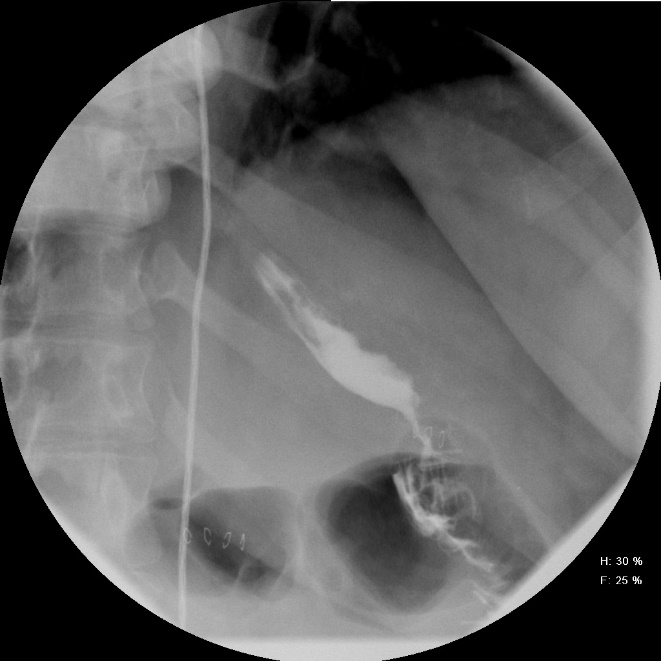

Post-op Bariatric UGI

Later that day, Ms. Montoya is instructed on the strict diet she must follow and discharged with an appointment to follow-up with Dr. Wheeler in three months.
Stop here!
Identify important observations and generate hypotheses based on your observations. Using numbers or arrows (or some other system), link each hypothesis to the observation(s) which support that hypothesis. What assessments/interventions should occur next in Ms. Montoya’s care?
Add to your list of learning issues.
At her three-month follow-up appointment, Ms. Montoya tells Dr. Wheeler that she has been having sharp pains on the right side of her abdomen for the last several days. The pain happens about 45 minutes to an hour after she eats.
History and Assessment
|
Vital Signs
|
Immediate Assessment:
- Initial wt: 416#
- Δ wt: 98#
- Assess for cholangitis
- Prophylactic Actigall 300 twice daily
- 6 mo. Follow up.
The patient services rep helps Ms. Montoya schedule a Nuclear Medicine study to evaluate the pain she has been having and informs her that the prescription for Actigall has been called in to her preferred pharmacy. Her 6-month follow-up appointment is scheduled.
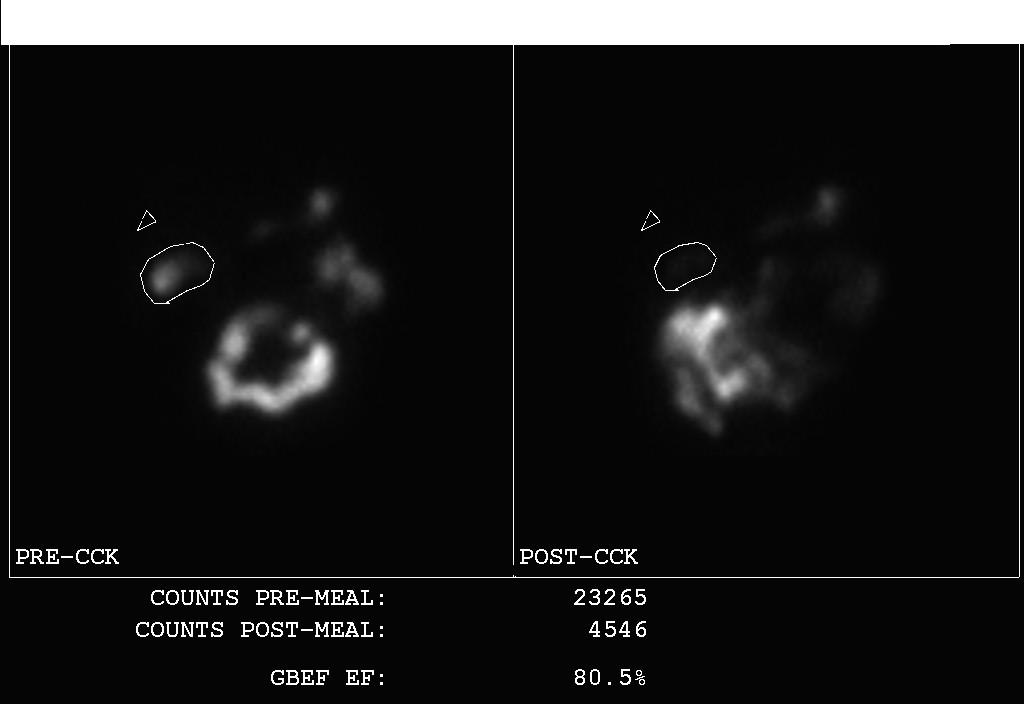
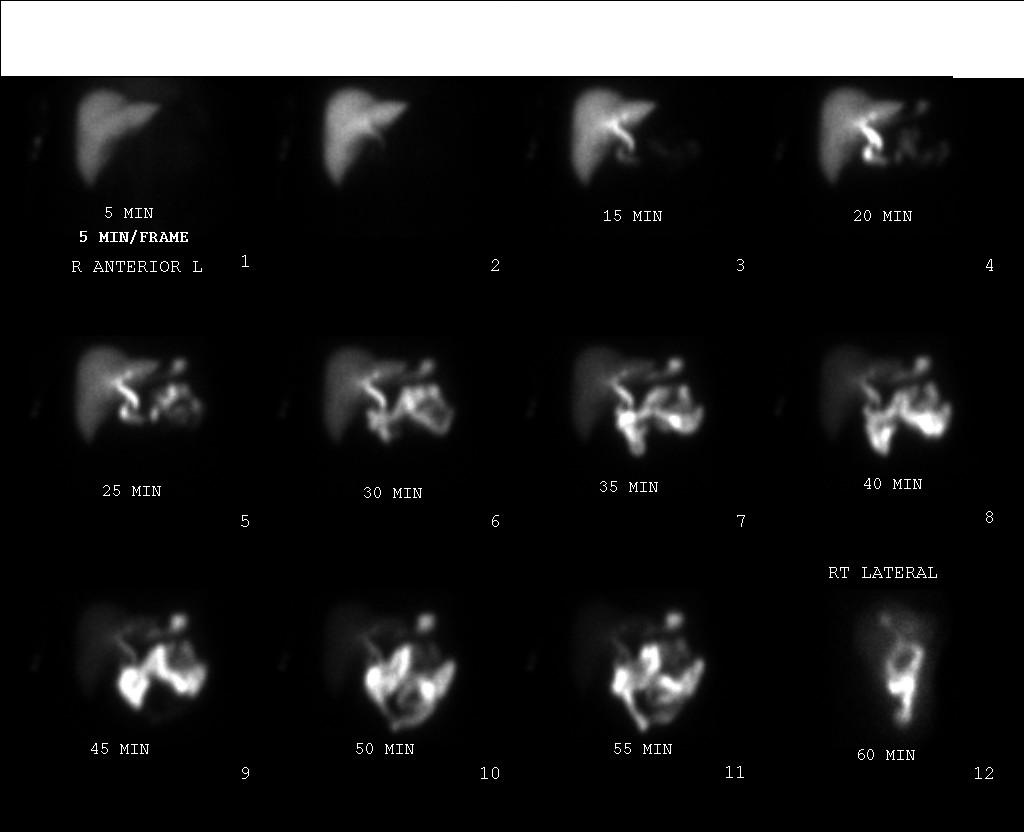
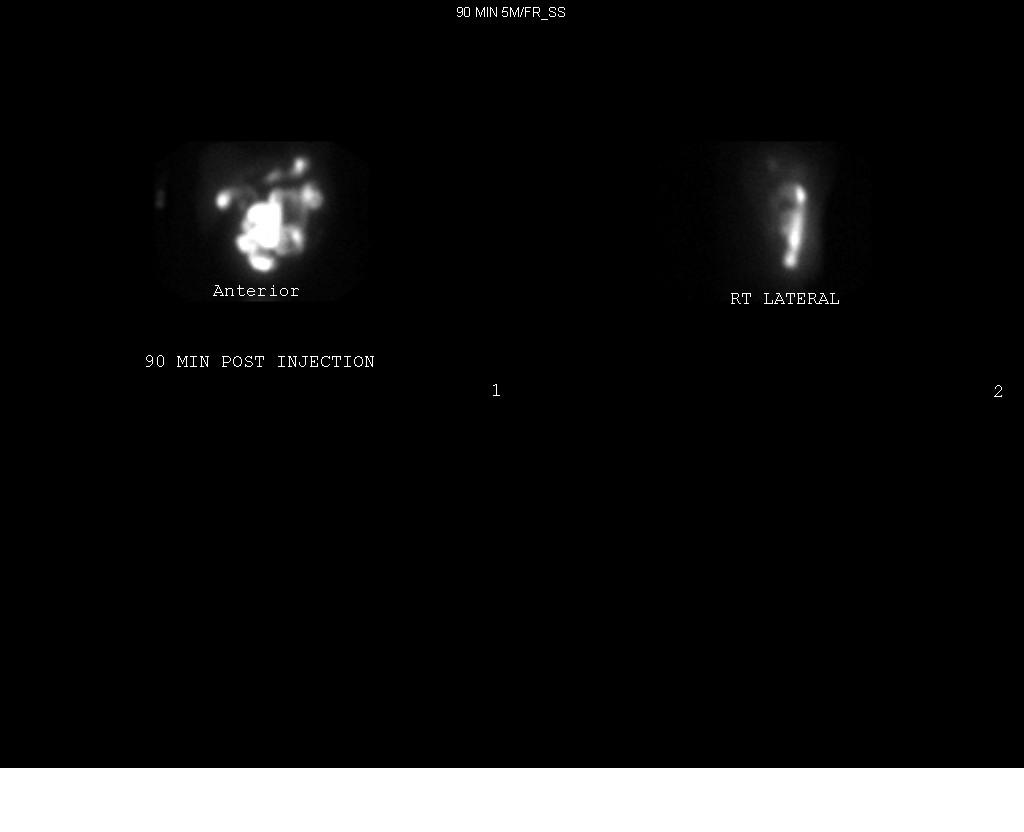
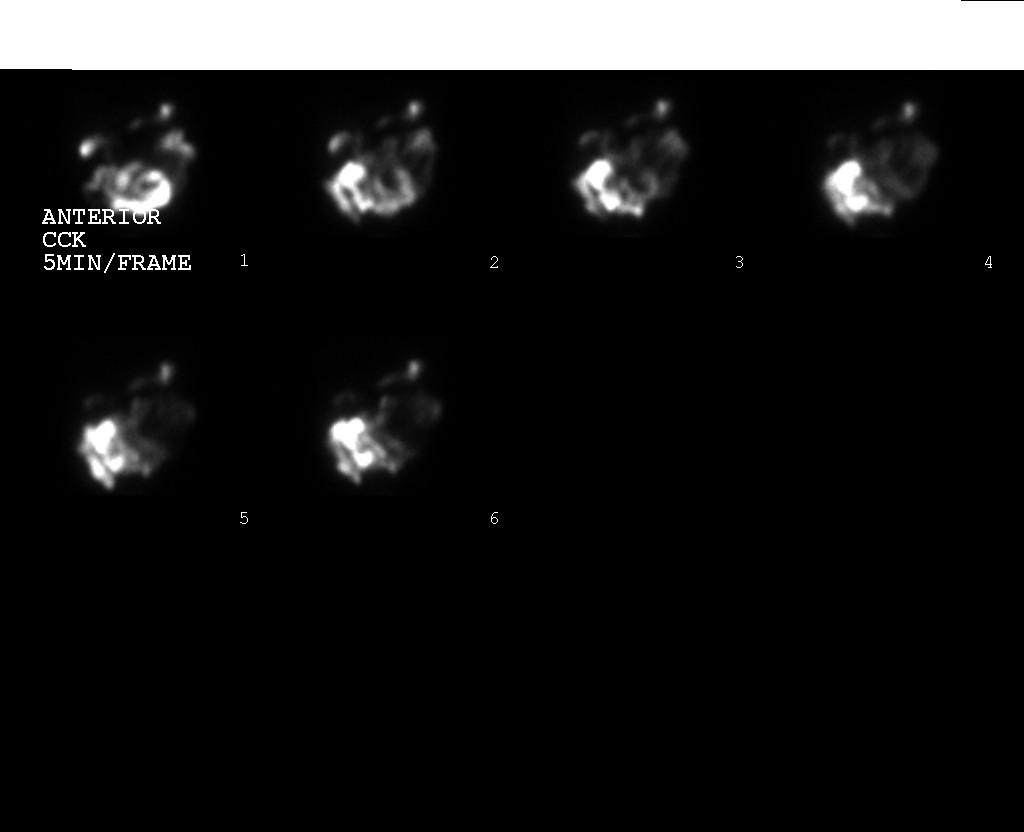
Nuclear Medicine Report
PROCEDURE: HEPATOBILIARY IMAGING STUDY AND GBEF
CLINICAL DATA: S/P BARIATRIC SURGERY WITH WEIGHT LOSS OF 150LB, POST PRANDIAL RUQ PAIN, NON-DIAGNOSTIC ABDOMINAL US
RADIOPHARMACEUTICAL: Tc-99m-MEBROFENIN (DOSE IN mCi: 7)
TECHNIQUE: THE RADIOPHARMACEUTICAL WAS INJECTED IV AND ANTERIOR IMAGES WERE TAKEN FOR ABOUT 90 MINUTES. RIGHT LATERAL IMAGES WERE ACQUIRED.
FINDINGS: THERE IS VISUALIZATION OF THE GALLBLADDER AND COMMON BILE DUCT. THE RADIOTRACER PASSES INTO THE DUODUNUM WITHOUT OBSTRUCTION. THERE IS MILD ENTEROGASTRIC REFLUX.
WITH THE GALLBLADDER FULL OF RADIOACTIVITY, THE PATIENT WAS INFUSED A DOSE KINEVAC (CCK) INTRAVENOUSLY OVER 20-30 MINUTES THROUGH AN INFUSION PUMP TO STUDY THE GALLBLADDER CONTRACTILITY AND EJECTION FRACTIONS. (NORMAL GBEF >35%).
THE GALLBLADDER EJECTION FRACTION IS 80%.
IMPRESSION: NEGATIVE FOR CYSTIC DUCT OR COMMON DUCT OBSTRUCTION. THE GALLBLADDER CONTRACTILITY IS NORMAL.
Stop here!
Identify important observations and generate hypotheses based on your observations. Using numbers or arrows (or some other system), link each hypothesis to the observation(s) which support that hypothesis. What assessments/interventions should occur next in Ms. Montoya’s care?
Add to your list of learning issues.
Ms. Montoya has her labs drawn before going to her 6-month follow-up appointment.
Lab Results – Metabolic Panel
| Test | Result | H/L | Ref Range Low | Ref Range High | UOM |
| Glucose | 94 | 57.0 | 110.0 | mg/dL | |
| BUN | 13 | 8.0 | 23.0 | mg/dL | |
| Creat | 0.7 | 0.7 | 1.6 | mg/dL | |
| Na | 141 | 134 | 145 | mmol/L | |
| K | 4.0 | 3.4 | 5.3 | mmol/L | |
| Cl | 104 | 101 | 113 | mmol/L | |
| Calcium | 9.6 | 8.4 | 10.2 | mg/dL | |
| Alk Phos | 59 | 20.0 | 108.0 | IU/L | |
| CO2 | 31.0 | 23.0 | 33.0 | mmol/L | |
| AST | 28 | 10.0 | 42.0 | IU/L | |
| ALT | 32 | 10.0 | 60.0 | IU/L | |
| TL Prot | 6.5 | 6.3 | 7.7 | Gm/DL | |
| Albumin | 4.4 | 3.5 | 5.0 | Gm/DL | |
| TBili | 0.9 | 0.1 | 1.3 | mg/dL | |
| OSMO | 281.1 | 269.0 | 302.0 | MOSM/L | |
| Anion Gap | 10.0 | 0.0 | 26.0 | ||
| BUN/Cre | 18.6 | ||||
| Chol | 101 | 130 | 240 | mg/dL | |
| Trigl | 70 | 39 | 190 | mg/dL |
Ms. Montoya tells Dr. Wheeler that she is feeling better than she has in years! Dr. Wheeler writes the following note.
History and Assessment
|
Vital Signs
|
Initial Assessment
- Initial wt: 416#
- Δ wt: 197#
Orders
- D/C Lexapro
- D/C Metformin
- D/C Lipitor
- Continue prophylactic Actigall 300 twice daily
- Schedule 12 mo. Follow up.
Stop here!This is the end of the case. Complete your list of important observations. Clarify your hypothesis list, adding and removing hypotheses on the basis of observations from the case. Link each hypothesis to the observation(s) which support that hypothesis. Finalize your list of learning issues. Determine the most important learning issues to your team. Assign learning issues and create focused clinical questions that address those learning issues.
Media Attributions
- normal-supine-trauma-chest-x-ray-in-an-obese-woman
- Lat CXR
- Diary Entry

