9 Case Analysis 4: Mrs. Spurlock’s Shoulder Pain
Learning Objectives
Process Learning Objectives:
Through authentic practice and shared inquiry in this case, students will develop:
- Information literacy skills, including the ability to locate, access, evaluate and use information in a wide range of situations.
- Awareness of the role of emotions in learning.
- Self-directed learning and metacognitive strategies to maximize their learning effectiveness.
- Fluency in reading, writing, summarizing, speaking, listening, viewing and presenting information.
- Social skills critical to effective team functioning, including interacting, cooperating, collaborating, and mutual respect for others’ ideas.
Content Learning Objectives:
Through authentic practice and shared inquiry in this case, students will develop a deep understanding of ceacute coronary syndromes (MI, heart attack) including:
- The risk factors for acute coronary syndromes, including ethnic and gender differences. Explain why each risk factor may lead to ACS.
- Common signs and symptoms of MI, including gender differences.
- The pathophysiology of acute coronary syndromes. Explain how and why acute coronary syndromes occur.
- The drugs used to respond to acute coronary syndrome, including their mechanism of action and why they are selected.
- The differential diagnosis of life-threatening chest discomfort.
- The various reperfusion options for ACS.
- How lab values are used to assess acute coronary syndrome. Explain which tests are most useful and how the positive result compares to the normal range.
- How Nuclear Medicine Stress Testing is used to evaluate patients with suspected MI, comparing positive images to normal ones. Identify cardiac anatomy.
- The process of preventing future cardiac events in patients with a history of AMI. Explain the types of pharmacologic intervention and how they work. Include non-pharmacologic (lifestyle) interventions as well.
- EKG changes that may indicate myocardial infarction and ischemia.
The Mystery of Mrs. Spurlock’s Shoulder Pain
Family Care Clinic
Mrs. Roseanne Spurlock, a 42 year-old caucasian woman, is returning to her family practice clinic for a visit. Her last visit was over a year ago. In the past few weeks, she has been experiencing fatigue and shortness of breath, and she has not been sleeping well. She takes care of her grandson because her daughter and son-in-law both work, and attributes much of her concerns to keeping up with him: “I think it’s just because Robert is such a busy boy! He’s two and has lots of energy! ” She reports that although she never seems to get enough sleep, she still has energy to cook for her family, do the shopping, and keep up the house. She notices mild shortness of breath when playing with her grandson at the park, which she attributes to her asthma. She has a history of mild asthma since childhood and occasionally uses an albuterol inhaler. She has never taken steroids for her asthma. She never has shortness of breath while at rest and has never experienced any chest pain.
History and Assessment
|
Past Medical History
|
|
Family History Mrs. Spurlock is married, with 2 children, ages 22 and 15. Her daughter is married and lives close by. Her son lives at home. She is a homemaker and takes care of her grandson during the day. Both her parents have high blood pressure. Her father had a heart attack about 8 years ago when he was 54. Her father had to have surgery for his heart back then, but he’s doing ok now. Her mom and brother have diabetes and are trying to eat better. She has had no changes in her weight. She reports her appetite is fair. Neither she nor her husband smoke. Her son-in-law is a smoker, but he is only allowed to smoke outdoors. |
Immediate Assessment
- Ht 5’4”
- Wt 226#
- BP 144/90 mmHg
- Pulse 86/min
- Respiratory rate 23/min
Current Medications
- Captopril 25 mg, 3 times daily
- Atenolol 50 mg, once daily
- Pravastatin 40 mg, once daily
- Metformin IR 500 mg, once daily
- Albuterol inhaler, as needed
The primary care physician agrees that Mrs. Spurlock’s complaints are probably due to her lack of sleep and exertion with her grandson and suggests that Mrs. Spurlock try an over-the-counter sleep aid to help with the insomnia. She is instructed to return to the clinic if her symptoms don’t improve.
Emergency Department
About 2 weeks after her visit to her doctor, Mrs. Spurlock arrives at the ED by private car. She is complaining of upper back pain that began early Saturday morning. She states that she thought she could make it until Monday to see her family physician, but then realized that she would need to wait until Tuesday because of the holiday weekend. The pain continued to worsen until it was causing her difficulty with breathing. Her daughter convinced her to come to the ED after church today. They arrive at the ER at 2:15 PM and are immediately shown to a treatment room.
Nurse Sarah obtained vital signs, started an 18 ga. IV and placed Mrs. Spurlock on O2 at 2L/NC.
History and Assessment
Immediate Assessment
- Ht 5’4”
- Wt 226#
- Temp 98.5º F
- BP 160/102 mmHg
- Pulse 82/min (regular)
- Respiratory rate 23/min (unlabored)
- O2 98% RA
Stop here!
Identify important observations and generate hypotheses based on your observations. Using numbers or arrows (or some other system), link each hypothesis to the observation(s) which support that hypothesis. What assessments/interventions should occur next in Ms. Spurlock’s care?
Begin your list of learning issues.
Dr. Clayton, the emergency room attending physician, performs an initial assessment.
History and Assessment
|
Past Medical History Mrs. Spurlock has a history of hypertension, asthma, diabetes and hyperlipidemia. Mrs. Spurlock is currently taking Captopril 25 mg TID, Atenolol 50 mg QD, Pravastatin 40 mg QD, Metformin IR 500 mg QD, and Albuterol inhaler 2-4 puffs PRN. |
|
Family History Mrs. Spurlock’s father has a history of heart trouble and high blood pressure. Her mother and brother have a history of diabetes. Social History Mrs. Spurlock denies alcohol or tobacco use. She is married and does not work outside the home, although she babysits for her grandson during the day. |
Physical Examination
- EENT: Eyes normal upon inspection
- Neck: Normal with no thyromegaly or lymphadenopathy
- Respiratory: No respiratory distress, chest non-tender, normal breath sounds.
- CVS: Regular rate and rhythm. No murmur, gallop or rub.
- Abdomen: Non-tender and no organomegaly.
- Skin: Normal color without rash; is warm and dry to touch.
- Extremities: Non-tender; normal ROM; no pedal edema; no calf tenderness.
- Neuro/Psych Mrs. Spurlock is oriented x 3. Her mood/affect are normal. CN’s normal as tested. No motor/sensory deficit.
Dr. Clayton orders a cardiac panel, STAT 12-lead EKG and a portable chest x-ray at 14:17. Nurse Sarah is drawing blood for the lab tests as the ECG Tech arrives and applies the leads for the 12-lead EKG.
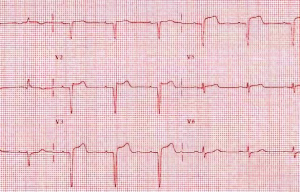
ECG FINDINGS
Vent rate 70 bpm Normal sinus rhythm
PR interval 160 ms ST elevation consider anterior wall injury or infarct
QRS duration 80 ms ** ** ACUTE MI ** **
Stop here!
Identify important observations and generate hypotheses based on your observations. Using numbers or arrows (or some other system), link each hypothesis to the observation(s) which support that hypothesis. What assessments/interventions should occur next in Ms. Spurlock’s care?
Add to your list of learning issues.
As the ECG Tech is removing the leads, Christie, the Radiologic Technologist, arrives with the portable x-ray machine to complete the chest x-ray.

Radiology Report
Examination: XR Chest Portable-PORTABLE
History: Dyspnea
Findings: Single AP image of the chest. No comparison available.
Borderline cardiomegaly. Pulmonary vasculature within normal limits. No pneumothorax, effusion, or focal infiltrate. Bony thorax unremarkable.
Impression: Negative for acute pathology
Dr. Clayton is informed of the ECG findings. She calls for a Cardiology consult and oversees the administration of the following emergency drugs:
- Plavix 300 mg initiated at 14:25.
- ASA 81 mg x 4 initiated at 14:25.
- IV Nitroglycerin Titrate 10mcg/min initiated at 14:25. –Pain rated at 6 on a one-to-ten scale with 10 as the worst pain ever.
- NTG increased to 20 mcg.min/6cc/hr. – Pain is unchanged.
- Lovenox 30 mg IVP initiated at 14:28. – Symptoms are unchanged.
- Zofran 4mg IVP initiated at 14:29 – Symptoms are unchanged.
Mrs. Spurlock’s lab results are back.
Laboratory Results
*** Chemistry ***
| Test | Result | H/L | Ref Range Low | Ref Range High | UOM |
| Glucose | 105 | 70.0 | 115.0 | mg/dL | |
| BUN | 7.0 | 7.0 | 18.0 | mg/dL | |
| Creat | 0.6 | 0.6 | 1.3 | mg/dL | |
| Na | 140.0 | 134.0 | 148.0 | mmol/L | |
| K | 3.5 | 3.5 | 5.1 | mmol/L | |
| Cl | 104.0 | 101 | 111 | mmol/L | |
| Calcium | 8.0 | L | 8.5 | 10.1 | mg/dL |
| CO2 | 24.0 | 22.0 | 29.0 | mmol/L | |
| Anion Gap | 12.00 | 0.0 | 26.0 | ||
| BUN/Cre | 12 | ||||
| CPK MB Fract | 6.0 | H | 0.5 | 3.6 | ng/mL |
| Troponin I | 0.37 | H | 0.0 | 0.05 | ng/mL |
| Myoglobin | 804 | H | 10 | 92 | ng/mL |
| CPKMB Reference Range | Troponin I Reference Range | Myoglobin |
| 0-10 ng/mL normal | 0.04 ng/mL apparently healthy | Expect values for normal PT < 116 ng/mL
Levels will start to increase 2-4 hrs after AMI. Peaking in 8-10 hrs, and return to baseline after 24 hrs. |
| 10.1 – 20 ng/mL borderline
elevation |
0.4 ng/mL diagnostic cutoff for AMI | |
| > 20 ng/mL elevated | <0.16 ng/mL elevated |
*** Coagulation ***
| Test | Result | H/L | Ref Range Low | Ref Range High | UOM |
| APTT | 25.8 | 23.9 | 35.1 | sec | |
| PT | 13.1 | 10.8 | 13.6 | sec | |
| INR | 1.14 | 0.7 | 1.3 | sec |
Her STAT 12-lead ECG shows an acute MI and her CXR is essentially unremarkable, except for borderline cardiomegaly.
Stop here!
Identify important observations and generate hypotheses based on your observations. Using numbers or arrows (or some other system), link each hypothesis to the observation(s) which support that hypothesis. What assessments/interventions should occur next in Ms. Spurlock’s care?
Add to your list of learning issues.
The Cardiologist sends Mrs. Spurlock to the Cardiac Cath Lab.
 |
 |
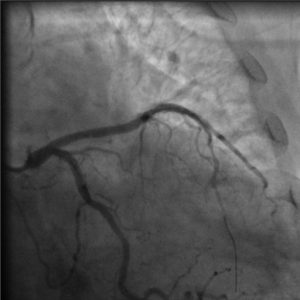 |
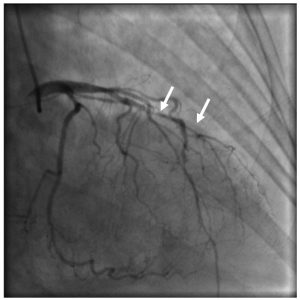
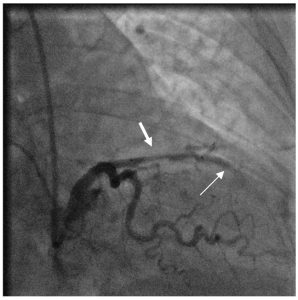
| Pre Intervention | During Intervention | Post Intervention |
Cardiovascular Catheterization Comprehensive Report
Patient name: Roseanne Spurlock
Age: 42
Gender: Female
Race: Caucasian
Procedure status: Urgent
Indications: -Angina/MI: myocardial infarction with ST elevation (STEMI), with onset less than 6 hours before admission.
-Coronary artery disease: suspected.
History: -The patient has history of asthma.
-The patient has insulin-controlled diabetes.
-The patient has hypertension, dyslipidemia
-There was no history of cerebrovascular disease, peripheral vascular disease, or renal failure. There is a family history of coronary artery disease.
Prior diagnostic test results: -Pre-procedure lab data: serum creatinine: 0.6 mg/dl.
Procedure: The risks and alternatives of the procedures and conscious sedation were explained to the patient and informed consent was obtained. The patient was brought to the cath lab and placed on the table. The planned puncture sites were prepped and draped in the usual sterile fashion. The procedure was performed urgently. Coronary intervention performed urgently.
-Right femoral artery access.
-Right and left coronary angiography.
-Left heart catheterization. Ventriculography was performed using power injection of contrast agent.
-Hemostasis w/ Angioseal.
Cardiac interventions
-Coronary Stent Placement.
Lesion #1 intervention: A stent was performed on the 90% lesion in the mid LAD. Following intervention there was a 0% residual stenosis. This was an ACC/AHA type B “moderate risk” lesion for intervention. There was TIMI 3 flow before the procedure and TIMI 3 flow after the procedure. There were no site complications. There was no acute vessel closure. There was no perforation. There was no dissection.
-Vessel setup was performed. A BMW Straight 0.014 x 300cm wire was used to cross the lesion. A XBLAD4.0 Guide 6F x 100cm guiding catheter was used to intubate the vessel. Balloon angioplasty was performed, using a Sprinter OTW 2.50 X 12mm balloon, with 1 inflations and a maximum inflation pressure of 6 atm. A Cypher OTW 3.00 x 18mm sirolimus-eluting stent was placed across the lesion and deployed with one inflation at a maximum inflation pressure of 14 atm.
Lesion #2 intervention: A stent was performed on the 80 % lesion in the distal LAD. Following intervention there was a 0 % residual stenosis. This was an ACC/AHA type B “moderate risk” lesion for intervention. There was TIMI 3 flow before the procedure and TIMI 3 flow after the procedure. There were no site complications. There was no acute vessel closure. There was no perforation. There was no dissection.
-Balloon angioplasty was performed, using a Sprinter OTW 2.50 X 12mm balloon, with 2 inflations and a maximum inflation pressure of 6 atm. A Cypher OTW 2.50 x 23mm sirolimus-eluting stent was placed across the lesion and deployed with one inflation at a maximum inflation pressure of 13 atm.
Procedure completion:
Timing: Test started at 14:42. Test concluded at 16:13.
Medications given: Midazolam, 1 mg, IV, at 14:49. Fentanyl, 25 mcg, IV, at 14:49. Midazolam, 1 mg, IV, at 15:58. Fentanyl, 25 mcg, IV, at 15:58. Nitroglycerin, 200 mcg, intracoronary, at 15:05. Nitroglycerin, 200 mcg, intracoronary, at 15:05. Nitroglycerin, 0.4 mg, SL, at 16:03. Heparin, 5,000 units, IV, last dose at 15:18. Eptifibatide (Integrilin), 7.9 ml, IV, last dose at 15:27. Eptifibatide (Integrilin), 14, IV, last dose at 15:28.
Contrast given: Visipaque 250 ml. Radiation exposure: Fluoroscopy time: 14.83 min.
Ventricles: -Analysis of regional contractile function demonstrated apical akinesis. EF calculated by contrast ventriculography was 40 %.
Coronary vessels: -The coronary circulation is right dominant.
-Left main: Normal.
-LAD: Angiography showed minor luminal irregularities.
-Mid LAD: There was a 90% stenosis. There was TIMI grade 3 flow through the vessel (brisk flow).
-Distal LAD: There was a 80% stenosis. There was TIMI grade 3 flow through the vessel (brisk flow). There was a 60% stenosis.
-Circumflex: Angiography showed minor luminal irregularities.
-1st obtuse marginal: There was a 30% stenosis.
-RCA: Angiography showed minor luminal irregularities.
Complications: No complications occurred during the cath lab visit.
Recommendations
-The patient’s medication regimen should include statin therapy, beta blockers, ACE inhibitors and nitrates.
-A Myocardial Perfusion SPECT study should be performed in 1 week.
Stop here!
Identify important observations and generate hypotheses based on your observations. Using numbers or arrows (or some other system), link each hypothesis to the observation(s) which support that hypothesis. What assessments/interventions should occur next in Ms. Spurlock’s care?
Add to your list of learning issues.
Mrs. Spurlock is kept overnight for observation following the catheterization procedure and discharged the next morning.
She was instructed to return in one week to undergo Nuclear Medicine Stress Testing. She was reminded to call if he had any recurrence of chest discomfort, shortness of breath, problems with her groin access site, or with any other concerns or questions.
Discharge Medications
- Captopril 25 mg, 3 times daily
- Atenolol changed to Metoprolol succinate 100 mg daily
- Asprin 81 mg daily was added
- Clopidogrel 75 mg daily for 6 months was added
- Nitrogard tabs buccal 1mg, every 3-5 hrs as needed
- Pravastatin 40 mg, once daily
- Metformin IR 500 mg, once daily
- Albuterol inhaler, as needed

Nuclear Medicine Report
PROCEDURE: MYOCARDIAL PERFUSION SPECT-PHARMACOLGIC
Age & History: 42 YOF; to assess myocardial viability following cardiac cath. History of CAD
Radiopharmaceuticals: For resting study, the patient was injected with 30 mCi of Tc-99m tetrofsomin intravenously. For stress images, the patient was injected with 30 mCi of Tc-99m tetrofosmin intravenously on a separate day from rest study.
For pharmacologic stress, the patient was given adenosine infusion as per protocol. Tc-99m tetrofosmin was injected during this infusion.
SPECT images were reconstructed in three dimensions.
Findings: There is a small 1+ anteroseptal reversible defect. No other reversible or fixed defects are noted on the myocardial perfusion images.
Impression: A small 1+ anteroseptal reversible defect. Differential diagnosis: attenuation artifact vs. CAD. Clinical correlation recommended. Likelihood of this being an artifact is high due to body habitus.
PROCEDURE: LEFT VENTRICULAR WALL MOTION, LV EJECTION FRACTION (LVEF)
Left ventricular functional assessment was performed from perfusion imaging described above. The images were gated and were acquired at least 15 minutes post-stress injection of Myoview. Computer analysis of this data was done to calculate left ventricular ejection fraction and to assess wall motion. (Normal LVEF >50%).
LVEF 69% and is normal.
Wall motion: Normal.
* * *Final Report* * *
Media Attributions
- Spurlock ECG
- Spurlock CXR
- Spurlock Cath Pre
- Spurlock Cath During
- Spurlock Cath Post
- Spurlock NM Stress

