5 mA, time and mAs
Before each and every x-ray exposure the radiographer has to set certain exposure factors on the control panel. How these factors are set determines the finished quality of the radiograph, as well as the radiation dose to the patient, so their proper selection is very important. If the radiograph has to be repeated because the exposure factors were selected improperly, the patient gets an unnecessary extra dose of radiation.
In this chapter you are going to learn about two of the primary exposure factors: milliamperage and exposure time, and their relationship to the quality of the IR exposure, patient dose and the four image properties. You will do some calculations of the mAs, which is a unit derived by combining milliamperage and exposure time. You will also learn how to manipulate the mA and time according to the reciprocity law.
Learning Objectives
At the end of this chapter, you should be able to:
- Define mA and explain its relationship to IR exposure, the four image properties and patient dose.
- Define time and explain its relationship to IR exposure, the four image properties and patient dose.
- Define mAs and explain its relationship to IR exposure, the four image properties and patient dose.
- Describe the relationship of mA, time and mAs to contrast, recorded detail and distortion.
- Convert a time quantity expressed in milliseconds to either a fraction or a decimal equivalent and convert a time quantity expressed as a fraction or decimal to its equivalent in milliseconds.
- Calculate the mAs with the time stated in either fractions, decimals, or milliseconds.
- Given two of these factors: mA, time or mAs, calculate the unknown factor.
- Change the mA, time or mAs in order to control IR exposure.
- Describe the reciprocity law by explaining how two different sets of mA and time settings can equal the same mAs.
- Use the reciprocity law to control motion, to use the small focal spot, and to use a breathing technique.
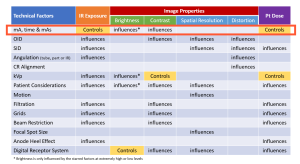
We are beginning our exploration of the technical factors that radiographers employ in creating the radiographic image with a discussion of milliampere-seconds, mAs. The mAs used in an exposure directly controls the image receptor exposure and patient dose and influences the contrast, and, to a lesser extent, the brightness seen on the displayed image. See Figure 5-1.
Figure 5-1
IR Exposure
In Chapter 4, we discussed the four image properties of brightness, contrast, spatial resolution and distortion, and the significant role that the exposure reaching the image receptor plays in these image properties. Recall that receptor exposure is expressed numerically as the Exposure Index. The EI (exposure index) is defined as a measure of the amount of x-ray photons reaching the image receptor in the relative image region. The exposure index value controlled by the amount or quantity of x-rays used to produce the image. The EI will be higher if a larger amount of x-rays is used to produce it.
Key Takeaways
Milliamperage
Two exposure factors directly control the quantity of x-rays produced and therefore the image receptor exposure. These are milliamperage and exposure time.
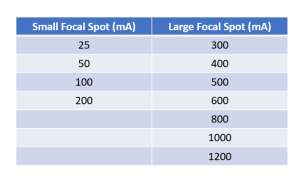
The milliamperage, or mA, is a measure of current passing through the x-ray tube at the time of the exposure. The milliamperage is set by the radiographer on the control panel and this setting determines the quantity of x-rays produced during the exposure. The mA setting determines how hot the filament of the x-ray tube gets. The heat of the filament controls how many electrons the filament releases, and the number of electrons released determines the amount of x-rays that are produced during an exposure. Figure 5-2 shows the typical mA settings available on control panels.
Figure 5-2: Typical mA Stations on a Control Panel
There is a nice, easy to understand direct relationship between the mA and the quantity of x-rays produced. If the mA is increased, the quantity of x-rays produced is increased, and if the mA is decreased, the quantity of x-rays produced is decreased. The relationship is so direct and dependable that if the mA is doubled, the amount of x-rays produced is doubled. If the mA is cut in half, the amount of x-rays produced is cut in half.
Key Takeaways
There is a Direct Relationship between mA and the quantity of x-rays produced.
- Increase in mA = Increase in the quantity of x-rays produced
- Decrease in mA = Decrease in the quantity of x-rays produced
The exposure to the image receptor is controlled by the quantity of x-rays in the beam. Since mA controls this quantity, there is also a direct relationship between mA and receptor exposure. If the mA is increased, the receptor exposure is increased, and if the mA is decreased, the receptor exposure is decreased. See Figure 5-3.
Figure 5-3: mA, X-Ray Quantity and Receptor Exposure
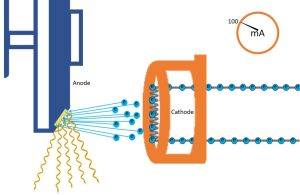
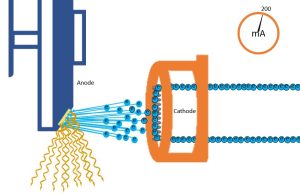
mA controls the number of electrons flowing through the filament per unit time. The number of electrons flowing determines the number of electrons released during thermionic emission. The number of electrons emitted from the filament controls the number of x-rays produced, and in turn the number of x-rays the patient and image receptor are exposed to.
Key Takeaways
There is a Direct Relationship between mA and the receptor exposure.
- Increase in mA = Increase in receptor exposure
- Decrease in mA = Decrease in receptor exposure
In clinical practice, it does not take many x-rays to produce an image of a small patient. A lower quantity of x-rays and therefore a small mA setting could be used. For a larger patient, the mA setting could be increased in order to increase the amount of x-rays. In routine radiography, using well-chosen techniques, milliamperage has no effect on contrast, recorded detail or distortion. The only thing the mA controls or changes is the quantity of x-rays produced, and that controls only the receptor exposure and the dose to the patient. mA cannot affect contrast because it does not change the energy of the x-rays in the beam. It changes the amount of x-rays equally in the entire beam, so as it produces more or fewer x-rays in the low-energy part of the beam, it also produces more or fewer x-rays in the medium or high-energy part of the beam. A change in the mA does not change any of the distances used during the exposure, or the image receptor system used, so mA cannot affect spatial resolution or distortion. It only changes the receptor exposure.
Key Takeaways
When employing well-chosen technical factors, the only thing mA changes is receptor exposure. At extremely high or extremely low mA levels the contrast will be affected.
Exposure Time
Another exposure factor the radiographer must set on the control panel before every x-ray exposure is the exposure time. The exposure time controls the length of the x-ray exposure by determining how long the current (mA) will be passing through the x-ray tube.
Key Takeaways
Since the mA controls the quantity of x-rays produced, the time also controls the quantity of x-rays produced because the time determines how long the mA will be working. Since mA has a direct relationship with receptor exposure, time also has a direct relationship with receptor exposure. If the time is increased, the exposure to the receptor will increase, and if the time is decreased, the exposure to the receptor with decrease.
Figure 5-4: Time, X-Ray Quantity and Receptor Exposure
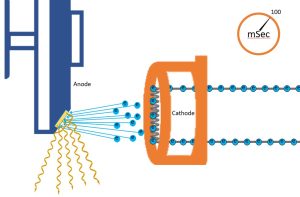
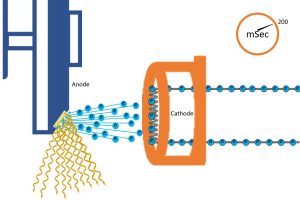
We can also control the number of x-rays created without changing the mA – we just let the electricity flow for a different amount of time. So, even though the same number of electrons are flowing through the filament per second, by varying the time, we can increase or decrease the number of electrons that are thermionically emitted from the filament, and subsequently, the number of x-rays that are created at the anode. If we change the number of photons created, the exposure to the patient and the image receptor will change.
Key Takeaways
There is a Direct Relationship between time and the receptor exposure.
- Increase in time = Increase in receptor exposure
- Decrease in time = Decrease in receptor exposure
As the time is increased, the exposure to the receptor increases. If the time is doubled, the exposure to the receptor doubles, if you cut the time in half, the exposure to the receptor is cut in half.
You have already learned the in routine radiography, using well-chosen techniques, mA controls the receptor exposure and does not affect contrast, spatial resolution or distortion. Since time controls how long the mA is working, it is easy to see that time also controls only the receptor exposure and does not affect contrast, spatial resolution or distortion.
If the exposure to the image receptor needs to be adjusted, either the mA or time can be changed. In clinical practice, it is better to change the time than the mA in order to change receptor exposure. You will see the reason for this later.
Time stations
Time stations on a control panel can be stated in milliseconds, decimals or, less commonly, fractions depending on the type of x-ray unit and the manufacturer. Most people are familiar with calculations involving fractions and decimals, but milliseconds may be a new term.
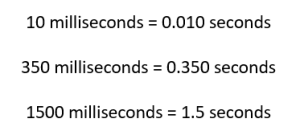
Milliseconds need to be converted to a fraction or decimal in order to perform calculations. The prefix “milli-” in front of a word changes it to 1000 times smaller. A millisecond is 1000 times shorter than a second. One thousand milliseconds equals 1 second. To change milliseconds to a fraction, put the number of milliseconds in the numerator and 1000 in the denominator.
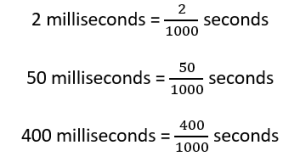
To change milliseconds to a decimal, put a decimal point to the right of the number of milliseconds, move it three places to the left and fill in any empty spaces with zeros. The thousandth place in the decimal system is the third place, which is why the decimal place is moved three places.
Activity 5A – Milliseconds
Milliampere-Seconds
If the two exposure factors of mA and time are put together they form a new unit called millampere-seconds (mAs). The mAs represents the total quantity of x-rays produced in an x-ray beam because it takes into account both the quantity of x-rays produced by the mA and the length of time the x-rays are produced.
Key Takeaways
mAs represents the total quantity of x-rays produced in a beam.
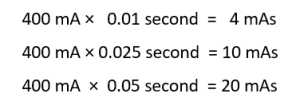
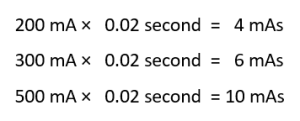
The mAs is the product of the mA and time and is calculated by multiplying the mA by the time.
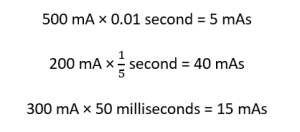
Be careful! When time is stated in milliseconds, the millisecond number must always be converted to seconds before it is multiplied by the mA.
Key Takeaways
On some control panels, technologists must set only the mAs and do not select the mA and time separately. On others, the mA and time are selected separatedly and the mAs is not shown. The mAs is not known until it is calculated. Some technologists perfer to think in terms of mA and time and others prefer to think in terms of mAs. Students need to become adept with both ways of thinking.
Activity 5B – Calculation of mAs
mA and time control only receptor exposure and do not affect contrast, spatial resolution or distortion. So the unit of mAs, composed of mA and time, also controls only receptor exposure and does not affect contrast, spatial resolution or distortion. There is a direct relationship between mA and receptor exposure and time and receptor exposure. So there must also be a direct relationship between mAs and receptor exposure. If the mAs changes, the receptor exposure must also change. If the mAs is decreased by 30%, the receptor exposure will be decreased by 30%.
Key Takeaways
There is a Direct Relationship between mAs and the receptor exposure.
- Increase in mAs = Increase in receptor exposure
- Decrease in mAs = Decrease in receptor exposure
Activity 5C – mAs Calculation with the Same mA or Time
Changing the Receptor Exposure with Milliampere-Seconds
If the receptor exposure needs to be changed because the image is overexposed or underexposed, totally new mA and time stations could be used for the repeated radiograph, or just the mA station or just the time could be changed.
If the mA station is kept the same and only the time is changed, a whole new mAs is produced and the exposure to the receptor will be changed.
If the time setting is kept the same and only the mA station is changed, a whole new mAs is produced and the exposure to the receptor will be changed.
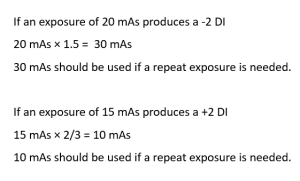
The direct relationship between receptor exposure and mAs is very useful in clinical practice. If a radiograph is overexposed and must be repeated, the technologist must decrease the receptor exposure. This is done very easily by decreasing the mAs, which can be accomplished by decreasing the mA or the time. If the radiograph is only slightly overexposed, having a DI of a little over +1, then the exposure is about 125% of the optimal exposure. If it is very overexposed, having a DI of over +3, the exposure is double the optimal exposure or more. To determine the degree of overexposure, you should look to the deviation index. If the DI is above +3, the mAs should be halved. If the DI is between +1 and +3, the mAs should be decreased by approximately 1/3. Recall that overexposed images should only be repeated if there are positioning error or the more radiolucent tissues are totally saturated. If the DI is below -3, the mAs should be doubled. If the DI is between -1 and -3, the mAs should be increased by 1/2.
Activity 5D – Calculation of the Unknown Factor
Reciprocity Law
Now here’s a dilemma. If the control panel is set at 500 mA and 0.02 seconds, 10 mAs would be produced. If it is set at 100 mA and 0.10 seconds, 10 mAs would also be produced. The total quantity of x-rays produced has not changed between the two different settings because the mAs is exactly the same. And the exposure to the image receptors should be exactly the same.
This is an example of the Reciprocity Law, which says that a variety of different mA and time settings could produce the same mAs and therefore the same receptor exposure. This law works well most of the time, except at very low or very high time frame settings. Here are some examples:
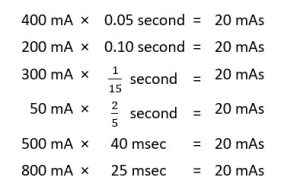
Key Takeaways
Technique charts usually show a specific mA and time setting that should be used on a body part. The charts ordinarily work well and can be depended upon most of the time. But a good radiographer also has the ability to use different settings from those the technique chart calls for depending on variables that can occur in clinical practice. There are three instances in clinical practice when the reciprocity law can be used. These are 1) to control motion, 2) to use a small focal spot, and 3) to use a breathing technique.
Control of Motion
If a patient moves during an x-ray exposure the radiograph will appear blurry. The recorded detail of the anatomy on the radiograph won’t be sharp and the radiograph would need to be repeated, causing more radiation exposure to the patient.
The possibility of motion blur on a radiograph can be reduced by using a short time setting on the control panel. For example, 300 mA and 0.5 seconds is 150 mAs. But 600 mA and 0.25 seconds is also 150 mAs. Two radiographs taken with these factors should have the same receptor exposure, but with the higher mA of 600 and the shorter time of 0.25 seconds, the patient would have less chance of moving during the exposure.
Key Takeaways
It is good practice to use a high mA station so that a short time can be used. This helps eliminate the chance of motion on the radiograph. It is often better in clinical practice to keep the high mA station and change the time rather than the mA when receptor exposure needs to be changed.
The Small Focal Spot
As learned in Ch. 1, the focal spot size is determined by which filament in the x-ray tube is heated. A small focal spot is achieved when the small filament is heated and a large focal spot is achieved when the large filament is heated. Heating of the different sizes of filaments causes either a small or a large area on the anode of the x-ray tube to be hit with electrons. This area on the anode is the actual focal spot.
The small focal spot is used to enhance spatial resolution. A small focal spot produces better recorded detail than a large focal spot, and this makes the image appear sharper.
Key Takeaways
On some x-ray control panels the radiographer must set the focal spot independent from the mA station. On other units, the focal spot and the mA station are both set at the same time because they are linked together on the same control panel button or dial. On both types of units the smaller mA stations produce a small focal spot and the larger mA stations produce a large focal spot. A small focal spot cannot be obtained with a high mA station.
A setting of 50 mA and 0.2 seconds will produce 10 mAs. This mA station would be in the small focal spot range; 500 mA and 0.02 seconds will also produce 10 mAs, but this high mA station would be in the large focal spot range.
The small focal spot cannot be used on every radiograph because the small filament cannot produce the higher mA that should be used for most of the radiographic exams that are performed. Chests, abdomens, spines, skulls and gastrointestinal (GI) work all require a high mAs and therefore a high mA station to produce enough receptor exposure because these are large body parts. Trying to heat the small filament and get a high mA can cause the filament wire to burn out and break.
In clinical settings the small focal spot is usually used on small body parts like hands, feet, wrists and noses. The small focal spot is used to enhance the recorded detail on these parts.
A smaller mA station is required when using the small focal spot. The ability to calculate the unknown factor in the formula mA x time = mAs is helpful here. First, figure out what mAs is necessary for the exposure. Then divide the mAs by the highest mA that is in the small focal spot range. The answer is the exposure time. If that time station is not available on the control panel, find an mA and time combination that will produce the mAs necessary and still use a small focal spot. This might take some trials before the right combination is found. The highest mA station that is in the small focal spot range should be used to keep the exposure time short and reduce the possibility of motion on the radiograph.
The Breathing Technique
How many times so far in your clinical education have you told patients to hold their breath? This is done to control the motion of the patient during the exposure. It prevents the image from becoming blurry due to the motion. The breathing technique flips this theory and purposely produced motion on a radiograph.
As the patient breathes, his or her ribs and lungs move. If a radiograph of the chest area is exposed while the patient is breathing, the ribs and bronchial markings of the lungs that are seen on chest radiographs would appear blurry. By purposely blurring these parts, the other structures in the chest area are seen better.
If a low mA station and long exposure time is used, the patient would have more opportunity to breathe during the exposure and blur out the ribs and bronchial markings. This special selection of a low mA with a long time is called the breathing technique.
Key Takeaways
Most radiographers use a breathing technique during sternum exams, and when performing a lateral projection of the thoracic spine. Also a transthoracic humerus radiograph, which is a lateral humerus exposed through the chest, is enhanced with the breathing technique. In these instances the sternum, thoracic spine and humerus are seen better because the ribs and bronchial markings of the lungs are blurred on the radiograph.
MAs and Contrast
This is important to remember when thinking about exposure factors. mAs does not affect contrast in typical diagnostic levels because mAs does nothing to the energy of the photons in the beam. It only changes the quantity of the photons produced. So mAs affects IR exposure by changing the total number of photons across the image receptor.
Summary
Milliamperage (mA) is the current in the x-ray tube at the time of the exposure. The exposure time determines how long the mA will be working. Time can be stated in fractions, decimals or milliseconds. mA multiplied by time forms a unit called mAs.
Time, mA and mAs determine the quantity of x-rays produced and the exposure to the patient and the image receptor. Time, mA and mAs are all directly proportional to image receptor exposure. They should be used to control receptor exposure. At normal exposure levels, they do not affect contrast, spatial resolution or distortion. At extremely high or low mAs levels, the image receptor may become saturated or may not receive sufficient photons to adequately create the image. At these levels, mAs will affect contrast.
The reciprocity law says that two sets of different mA and time selections can produce the same mAs. This allows the radiographer to manipulate the mA and time to control motion by using a short exposure time, use the small focal spot by selecting a low mA station, and use the breathing technique by selecting a long exposure time with a low mA.
- mAs is a technologist-controllable factor
- mAs and Exposure/Dose
- mAs’ impact on beam quantity exiting the tube
- mA, time and mAs are directly proportional to radiation exposure. (Remember – Exposure is the number of photons in the beam.)
- mAs Reciprocity – mAs is the product of mA and time. It doesn’t matter what the individual mA or time is, if the mAs is the same, the exposure is the same.
- mA, time and mAs are directly proportional to radiation exposure. (Remember – Exposure is the number of photons in the beam.)
- mAs’ impact on beam quantity exiting the tube
- mAs’ impact on beam quality exiting the tube
- Changes in mA, time or mAs do not change the penetrating energy of the beam.
- mAs and Signal Properties
- mAs’ impact on beam quantity exiting the patient
- mA, time and mAs are directly proportional to the Exposure Index.
- It doesn’t matter what the individual mA or time is, if the mAs is the same, the IE number will be the same.
- mA, time and mAs are directly proportional to the Exposure Index.
- mAs’ impact on beam quantity exiting the patient
- mAs’ impact on beam quality exiting the patient
- Changes in mA, time or mAs do not change the penetrating energy of the beam.
- mAs and Visibility Properties
- mAs’ impact on Brightness
- Changes in mA, time or mAs do not change the brightness of the image.
- mAs’ impact on Contrast
- mA, time and mAs changes only impact contrast at the far ends of the spectrum, when contrast differences become indistinguishable, i.e. the image features are no longer visible.
- mAs and Accuracy Properties
- mAs’ impact on Recorded Detail
- Changes in mA, time or mAs do not change geometric factors influencing recorded detail
- EXCEPT when uncontrolled movement is an issue, then shorter exposure times improve recorded detail.
- mAs’ impact on Distortion
- Changes in mA, time or mAs do not change the geometric factors influencing distortion.
- mAs’ impact on Recorded Detail
- mAs’ impact on Brightness
